The evaluation of a patient with a palpable solitary nodule is generally straightforward and usually will include a fine-needle aspiration (FNA) biopsy with or without US guidance.
The evaluation of a patient with a palpable solitary nodule is generally straightforward and usually will include a fine-needle aspiration (FNA) biopsy with or without US guidance. It is important to recognize that in up to 50% of patients with a clinically palpable solitary nodule, ultrasonography will often demonstrate the presence of one or more additional nodules.2 The evaluation and management of patients with multinodular goiters (MNGs) represents a much more difficult problem in the clinical setting. Non-palpable nodules have the same risk for malignancy as palpable nodules of a similar size.3 Although it has been generally postulated that the risk for thyroid cancer is lower in patients with MNG compared with patients with solitary nodules, some studies have shown a similar incidence of cancer in both groups.4,5
The clinical manifestations of patients with MNGs are variable and to a great extent depend on the size and location of the goiter and whether the nodules are hyperfunctioning or not. Many patients with MNGs can be completely asymptomatic, particularly when the goiter is small and the functional status of the thyroid is normal. Other patients may present with a visible goiter that may have been present for years in the absence of other clinical symptoms. However, in some patients thyroid growth may occur in the thoracic cavity (substernal goiters) and result in obstruction or pressure of any of the structures within the cavity. Tracheal compression can result in dyspnea, which is most commonly exertional but can be positional;6,7 dysphagia or hoarseness from compression of recurrent laryngeal nerve are other symptoms that may be seen in patients with large goiters. Hyperthyroidism, either overt or subclinical, may be present in up to 25% of patients with MNG.8 Diagnostic Evaluation
Serum Thyroid-stimulating Hormone
The initial evaluation of patients presenting with a nodular goiter should include a complete history and physical exam and measurement of serum thyroid-stimulating hormone (TSH) levels. If serum TSH levels are low, indicating overt or subclinical hyperthyroidism, the presence of hyperfunctioning (‘hot’) nodules is likely, and thyroid scintigraphy should be performed to determine the functional status of the nodules. As hot nodules are rarely malignant, such thyroid nodules would not require cytological evaluation.9 A higher TSH is often associated with chronic autoimmune (Hashimoto’s) thyroiditis and presents with apparent nodularity, which sometimes may represent focal lymphocytic infiltration (pseudo-nodules). US evaluation may be helpful in distinguishing these findings from true thyroid nodules. Recent studies have found serum TSH to be an independent risk factor for predicting malignancy in patients with thyroid nodules.10,11 In a study of 1,500 patients presenting for evaluation of thyroid nodules, the prevalence of malignancy increased from 2.8% when TSH was <0.4mU/l, to 3.7% for TSH between 0.4 to 0.9mU/l, and up to 29.7% when TSH was >5.5mU/l.10 In addition, another study showed that in patients diagnosed with thyroid cancer, a higher TSH was associated with a more advanced stage of the disease.11
Thyroid Scintigraphy
Scintigraphy is the standard method for functional imaging of the thyroid. In patients with a nodular goiter and suppressed serum TSH levels, thyroid scanning provides a measure of the iodine-trapping function in a nodule compared with the surrounding thyroid tissue. The sensitivity of 123I scanning is ~83%,12 whereas that of technetium scanning is ~91%.13 The specificity of thyroid scans is low—25% for radioiodine scans and 5–15% for technetium scans—and this low specificity is mostly because other thyroid lesions interfere with uptake of the radioisotopes. Due to its low diagnostic accuracy, the utility of thyroid scintigraphy in the evaluation of thyroid nodules is limited and, at present, its major role is in confirming the functional status of suspected autonomously functioning thyroid nodules.
Ultrasonography
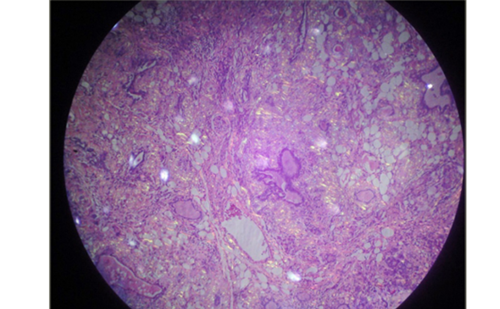
Current US technology, using high-resolution transducers, is an excellent method for detection of thyroid nodules as small as 1–2mm. Its sensitivity approaches 95%—better than other available methods, including radioisotope scanning, computed tomography (CT), and magnetic resonance imaging (MRI). Thyroid ultrasonography is increasingly being used as an extension of the physical examination, leading to an epidemic of thyroid incidentalomas. All patients with a nodular thyroid, either a palpable solitary nodule or MNG, should be evaluated with US.9,15 Ultrasonography is useful in confirming the presence of a mass, determining whether it is of thyroidal or extrathyroidal origin, assessing whether the lesion is single or multiple, and guiding FNA. As no single clinical or ultrasonographic feature has been found to reliably confirm or exclude the presence of malignancy, selection of the nodule(s) that require biopsy needs careful consideration. Certain ultrasonographic features of thyroid nodules, such as hypoechogenicity, the presence of microcalcifications, increased vascular flow, or irregular borders, are associated with increased risk for malignancy,4 and, when present, should help the clinician in selecting the target of the FNA biopsy (see Figure 1). Due to the fact that in the absence of these features malignancy cannot definitively be excluded, patients with MNGs should be followed by periodic neck examinations and ultrasonography, and a repeat biopsy should be considered if significant growth of a nodule is noted or there are other worrisome clinical (persistent hoarseness, dysphagia, adenopathy, etc.) or sonographic features develop on follow-up.
Ultrasonography is also helpful in the follow-up of patients with MNG to evaluate nodule growth, since a false-negative rate of up to 5% has been reported in patients with previous benign cytology.16,17 Although there is no consensus on the definition of ‘clinically significant growth’ of a thyroid nodule, the American Thyroid Association (ATA) task force guidelines define growth as a 20% increase in nodule diameter with a minimum increase of at least 2mm in two or more dimensions.9
Other Imaging Modalities
CT and MRI are not recommended for routine use in patients with thyroid nodules because of their high cost, but these imaging modalities can be valuable in assessing size, substernal extension, and positional relationship to surrounding structures, particularly in patients with large goiters, those with suspected substernal extension, and those with obstructive or pressure symptoms (see Figures 2 and 3). Fine-needle Aspiration Biopsy
This technique is the most accurate method for selecting patients needing thyroid surgery. Most centers utilizing FNA biopsy have achieved a 35–75% reduction in the number of patients requiring surgery, while still doubling or tripling the malignancy yield at thyroidectomy.18–20 Selection of nodules that require biopsy in patients with MNG may be challenging. With experience, adequate samples can be obtained in 90–97% of aspirations of solid nodules. As patients with MNG have the same risk for malignancy as those with solitary thyroid nodules,4,5 biopsy of the ‘dominant’ nodule only can often miss thyroid cancer.5 US guidance has proved extremely helpful in selecting the best targets for FNA, and is particularly valuable in small nodules (<1.5cm) and essential for non-palpable nodules, helping to ensure proper placement of the needle tip for precise sampling. In complex or cystic nodules, US guidance helps direct the needle tip to the solid component of those nodules, avoiding areas of central necrosis, which often yield inadequate specimens (see Figure 4).21 The management of biopsy-proven benign or malignant nodules is often straightforward with observation or surgical excision, respectively. However, nodules with indeterminate or ‘suspicious’ cytology continue to pose a clinical challenge given the lack of reliable markers to accurately predict the nature of such lesions. A thyroid scan has been recommended in these patients to evaluate for autonomous function. In the absence of autonomous function, surgical excision is recommended,9 even though ultimately only 15–20% of these lesions will prove to be malignant on final pathology.22,23 Nodules with inadequate or insufficient cytology (non-diagnostic) should be re-aspirated, preferably under US guidance. If repeat aspirations fail to provide an adequate specimen, close follow-up or surgery (particularly if the nodule is solid) should be considered.9
Treatment Options for Patients with Multinodular Goiters
Several treatment modalities are available for patients with MNGs. The selection of the best therapeutic option will depend on several factors, including goiter size, location, the presence and severity of compressive symptoms, and the presence or absence of thyrotoxicosis.
Thyroid-hormone-suppressive Therapy
As TSH is regarded as a growth factor for thyroid epithelial cells,24,25 treatment with levothyroxine in doses sufficient to suppress TSH has been used for years to prevent or reduce growth of thyroid nodules. However, the effectiveness of this practice remains controversial.26,27
A clinical trial of 78 patients with non-toxic goiter treated with levothyroxine or placebo for nine months and then followed up for an additional nine months showed a 58% reduction in goiter volume assessed by ultrasonography versus a 4% reduction in the placebo group, but this effect was lost after levothyroxine therapy was discontinued.28 A review of seven non-randomized trials of suppressive therapy for non-toxic goiter found that 60% of patients had some decrease in goiter size during thyroid hormone therapy.29 The decrease tended to occur in the first three months of treatment, and a better response was observed in those patients with diffuse rather than nodular goiters. The efficacy of levothyroxine suppressive therapy in preventing recurrence of goiter growth after partial thyroidectomy is less clear. Several non-randomized trials suggest that levothyroxine therapy is effective for this purpose, but randomized trials have failed to show a significant reduction in recurrence of goiter in these patients.30 However, some of these studies were small or of short duration, and some did not achieve adequate TSH suppression or showed a statistically non-significant trend toward fewer recurrences with levothyroxine therapy. It has also been suggested that in patients with MNG, levothyroxine therapy may prevent formation of new nodules by interfering with the process of goitrogenesis, even if it does not cause regression of the clinically apparent nodule.30 Due to the known risks associated with subclinical hyperthyroidism resulting from suppressive levothyroxine therapy, caution is warranted when considering this treatment option in post-menopausal women, particularly those with evidence of low bone mass, the elderly, and those with cardiac disease, in whom the risks of this therapy may be increased, particularly given the uncertainties about its efficacy.31,32
Radioiodine Therapy
Radioiodine (RAI) has been widely and effectively used for the treatment of toxic MNGs.33 Administered orally, usually as a single dose, it is rapidly concentrated in thyroid tissue and results in the destruction of toxic nodules over a period of two to four months. Some patients, particularly those with severe hyperthyroidism or large goiters, may require more than one dose to achieve euthyroidism. Radioiodine is preferentially accumulated in the hyperfunctioning nodules and, therefore, subsequent rates of hypothyroidism are much lower than in patients treated with RAI for Graves’ disease. Patients with severe thyrotoxicosis, particularly the elderly and those with cardiac history, are often pre-treated with antithyroid drugs (methimazole [MMI] or propylthiouracil [PTU]). There is evidence that PTU, but not MMI, may reduce the effectiveness of subsequent RAI therapy in these patients.32 Young and otherwise healthy patients do not need pre-treatment with antithyroid drugs. Although RAI has not traditionally been considered a treatment option for patients with non-toxic MNGs, several studies, mostly from Europe, have demonstrated that it is in fact both safe and effective.35–37 This treatment has the advantage of resulting in significant goiter size reduction (30–60%), most of which occurs within the first year after treatment,38–40 with improvement in obstructive symptoms (dyspnea, dysphagia) in most patients,38,39 and in one study RAI was shown to be more effective than levothyroxine therapy40 in reducing goiter size. Transient hyperthyroidism may occur in the first two weeks after RAI treatment, and permanent hypothyroidism has been reported in up to 45% of patients.40 Pre-treatment with recombinant human TSH (rhTSH) has been evaluated in recent years as adjuvant to RAI in several studies as a means to enhance the efficacy of RAI uptake in non-toxic thyroid tissue (in one study RAI uptake doubled),41 allowing the use of lower doses of RAI42 and enhancing goiter size reduction.41,43–46 Additionally, pre-treatment with rhTSH has been shown to modify the regional distribution of RAI by stimulating RAI uptake in relatively hypofunctioning regions within a goiter.47 Painful transient thyroiditis and transient mild thyrotoxicosis,43 usually within the first month after treatment, and increased incidence of subsequent hypothyroidism have been described. Additionally, an increase in goiter size with rhTSH is a potential concern, especially in patients with very large goiters in whom obstructive symptoms could be transiently worsened shortly after treatment.48 Development of Graves’ hyperthyroidism (with high levels of TSH-receptor antibodies) has been described after treatment with RAI in patients with MNGs and seems to be more common in those with high thyroid peroxidase (TPO) antibody concentrations before the treatment.49
Surgery
Patients with large, obstructive, and substernal non-toxic MNGs or those with continued growth are best managed with surgery if they have acceptable surgical risk. Complications of surgery for large and substernal goiters are more commonly seen than in patients undergoing thyroidectomy for cervical goiters50 and
nclude injury to the recurrent laryngeal nerves, trachea, and parathyroid glands.6 A study of nearly 34,000 patients who underwent thyroidectomy—of whom 1,153 (3.4%) had substernal thyroidectomy— showed that this last group of patients were older, more likely to have a comorbid condition, to be men, to lack private insurance, and to undergo total thyroidectomy, and less likely to undergo thyroidectomy for malignancy and to have this procedure performed at a high-volume center. Patients requiring surgery for substernal goiter should be referred to experienced surgeons in high-volume centers to minimize complication rates.51
Conclusion
The evaluation and management of patients with nodular goiters is frequently more difficult than that of patients with solitary thyroid nodules. There is consensus on the importance of serum TSH measurement as the initial step to exclude hyperfunctioning nodules (which have very low risk for malignancy) and the central role of ultrasonography and FNA biopsy (preferably under US guidance) when suspicious nodules are seen, to exclude malignancy. Continued follow-up with periodic US is helpful to evaluate for clinically significant growth of nodules that may warrant re-aspiration, and selection of nodules that warrant FNA biopsy should be guided by sonographic features, clinical history, and rate of growth. Although several treatment modalities are available for the management of patients with MNGs, the efficacy of some of these treatments, such as levothyroxine suppressive therapy, is less clear and the risk–benefit ratio of each option should be carefully discussed with patients. The advent in recent years of rhTSH and its potential applications52 appears promising, including its use in the pre-treatment of patients with nontoxic MNGs receiving RAI, allowing for the use of reduced doses of RAI with enhanced goiter size reduction. However, currently it is still not US Food and Drug Administration (FDA)-approved for this purpose and caution is warranted, particularly in elderly patients and those with large goiters and compressive symptoms. Furthermore, prospective controlled studies are needed to better define its value and clinical applications before widespread use can be recommended.