18F-fluorocholine-positron emission tomography/computerized tomography (FC-PET/CT) has traditionally been used for disease localisation and management in oncology (e.g. hepatocellular carcinoma and prostate cancer).1 Diagnosis of parathyroid adenomas incidentally picked up in patients with malignancy who underwent FC-PET/CT led to its evaluation in parathyroid imaging.2 A few recent reports have suggested the beneficial role of PC-PET/CT in localising culprit lesions (hyperfunctional parathyroids) in patients with primary hyperparathyroidism (PHPT) otherwise not localised with 99mTc-sesta-methoxyisobutylisonitrile (sestaMIBI) imaging and high-resolution neck ultrasonography.3 PC-PET/CT has been documented to be useful in localising parathyroid hyperplasia, and ectopic parathyroids, which are often missed by the more traditional reference test, sestaMIBI imaging.4 Parathyroid cysts are very rarely associated with PHPT, which are difficult to localize, as they are sestaMIBI negative.5 We report for the first time the utility of PC-PET/CT in localising parathyroid cyst causing normocalcemic PHPT in a postmenopausal lady with severe osteoporosis which was not responding to bisphosphonate therapy.
Patient report
A seventy-six-year-old lady who was 28 years postmenopausal, was diagnosed with osteoporosis in 2014 (see Table 1). Biochemical evaluation was significant for vitamin D deficiency with secondary hyperparathyroidism. Patient was started on calcium carbonate and cholecalciferol supplementation and received injections of zolindronic acid infusion (5 mg). Re-evaluation after 1 year revealed minimal improvement in bone mineral density (BMD) on dual energy X-ray absorptiometry (DEXA), normal serum 25-hydroxy-vitamin-D (25OHD) and elevated serum parathyroid hormone (112 pg/ml) (see Table 1). Ultrasonography and sestaMIBI imaging of the neck was normal (2015). Serum calcium and vitamin D remained normal, BMD continued to progressively worsen (in spite of annual zolendronic acid infusions) and parathyroid hormone remained elevated on repeated measurements from 2015–2017 (Table 1). SestaMIBI imaging was repeated twice in 2016 but failed to localise any parathyroid adenoma.
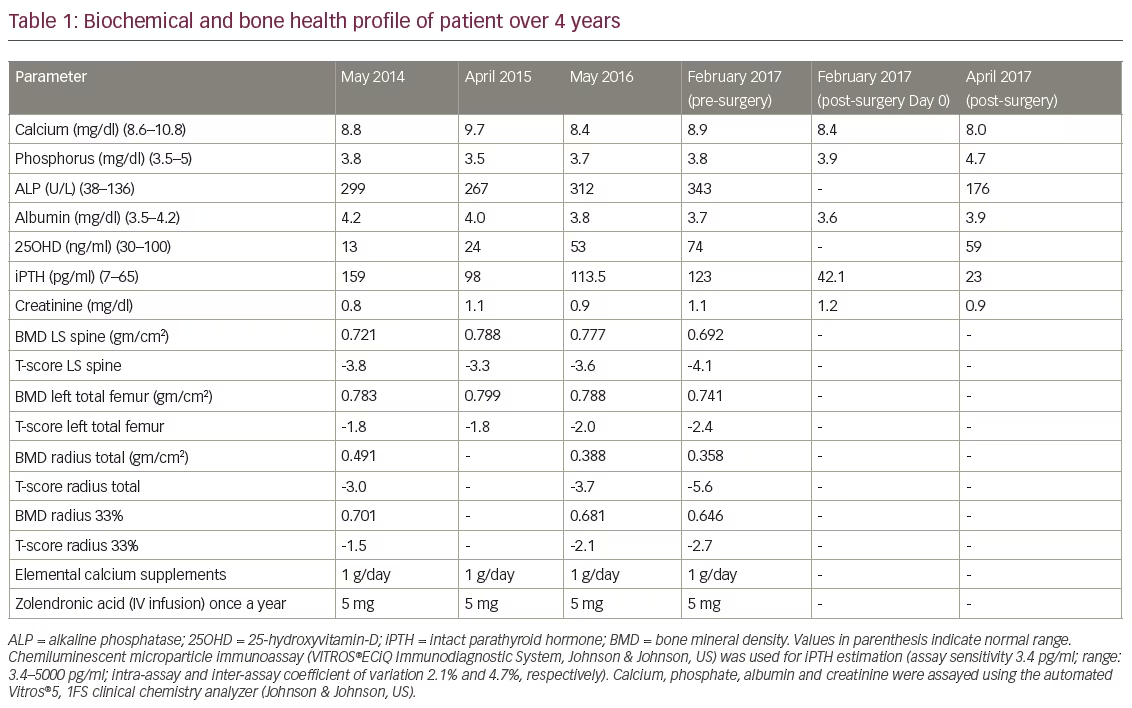
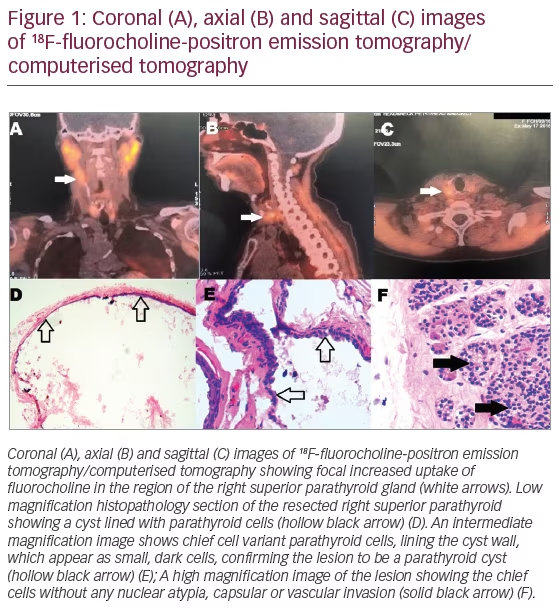
FC-PET/CT was done in May 2016 following injection of 5 mCi of 18F-fluorocholine by intravenous route. Computed tomography (CT) imaging was done from the orbits to the mid thorax region, revealed soft tissue uptake, posterior to the middle of the right lobe of the thyroid, extending superiorly for a cranio-caudal length of 1 cm, in close relation to the right lamina of the thyroid cartilage, 3 mm antero-medial to the right common carotid artery and 2 mm medial to the internal jugular vein, which was suggestive of right superior parathyroid adenoma/hyperplasia (Figure 1A–1C).
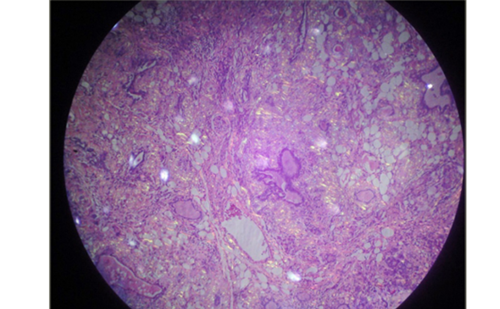
The patient was apprehensive about parathyroid surgery, leading to deferment of definitive surgical cure for primary hyperparathyroidism. However, with further worsening BMD in 2017, she finally agreed to neck surgery and underwent right superior parathyroidectomy, where a parathyroid cyst was removed. Her preoperative (on the day of surgery) and 20-minute post-parathyroidectomy iPTH were 123 and 42.1 pg/ml, respectively, indicating surgical cure of PHPT. Histopathology of surgical specimen revealed a cystic lesion lined by chief cell variant parathyroid cells without any nuclear atypia, capsular or vascular invasion (Figure 1D–1F). When last evaluated 2 months after the surgery, the patient was doing well, and was on calcium and cholecalciferol supplementation.
Discussion
Accurate preoperative localisation of the culprit parathyroid using sestaMIBI imaging is central to reducing morbidity associated with surgical management of primary hyperparathyroidism (reduced exploration and lesser complications). SestaMIBI can accurately localise 60–80% of single parathyroid adenomas, accounting for 75–80% of PHPT.6 Reasons for false negative of sestaMIBI and failure to localise the culprit lesion in primary hyperparathyroidism include extremely small adenomas, double parathyroid adenoma, ectopic parathyroid adenoma, parathyroid hyperplasia and parathyroid cysts.7 Parathyroid cysts are rare, with only 300 such cases being reported to date.8 Parathyroid cysts are usually non-functional.8 Functional parathyroid cysts are uncommon (observed in 30% of all parathyroid cysts), and contribute to 1% of all primary hyperparathyroidism.9 Parathyroid cysts account for <1% of neck masses and have a female preponderance (2.5:1).8 The genesis of parathyroid cysts are multifactorial and may include cystic degeneration in a parathyroid adenoma (infarction within adenoma), coalescence of microcysts with hypersecretion within the capsule of the gland or persistent embryological remnants of branchial cleft cysts.8,10
Failure to localise the culprit parathyroid, especially in the setting of normocalcemic hyperparathyroidism can lead to delay in the definitive surgical cure of the disease, which can lead to increased morbidity such as severe osteoporosis resistant to medical management,11 as was the case with our patient. Ultrasonography is a useful adjunct having 51–78% and 67–96% sensitivity and specificity, respectively, in localising parathyroid adenoma.7 However, its use is limited by inter-operator variability and it failed to localise the small parathyroid cyst in our patient. In sestaMIBI-negative primary hyperparathyroidism, if a suspicious lesion is seen on neck ultrasonography, fine-needle aspiration biopsy along with needle-tip parathyroid hormone greater than serum parathyroid hormone is a useful test in localising the culprit parathyroid.7,12
18F-fluorocholine is a metabolic tracer with increased uptake at any site of increased metabolic activity, explaining its positivity in the evaluation of cancers, inflammation and in benign lesions such as parathyroid adenomas/hyperplasia. A recent series of patient case studies demonstrated that PC-PET/CT is a useful tool for detecting hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism (7 parathyroid adenoma and 10 parathyroid hyperplasia).13 It may be hypothesised that the better resolution of positron emission tomography imaging as compared to scintigraphy and single-photon emission computed tomography, makes FC-PET/CT an attractive option for localising ectopic parathyroid adenomas and hyperplasia, especially in the mediastinum. However, there is an urgent need for comparative studies between sestaMIBI and FC-PET/CT in primary hyperparathyroidism, before PC-PET/CT can be recommended for routine use in the diagnosis of primary hyperparathyroidism. To conclude, it may be said that PC-PET/CT helped in localising the culprit parathyroid cyst causing primary hyperparathyroidism in our patient, resulting in surgical cure. This is the first report of PC-PET/CT use in localising a parathyroid cyst causing sestaMIBI-negative normocalcemic primary hyperparathyroidism.