Incidence
The incidence of thyroid cancer has been increasing in both men and women since 1976.1 It has been estimated that there will be 37,340 new cases of thyroid cancer in the US in 2008. Despite the increasing incidence of thyroid cancer, mortality rates have declined, leading to an estimate of 1,590 deaths from the disease in 2008.2 The opposite trends in incidence and mortality may be partially due to the fact that increased detection of small papillary cancers has significantly contributed to the overall incidence.3
Incidence
The incidence of thyroid cancer has been increasing in both men and women since 1976.1 It has been estimated that there will be 37,340 new cases of thyroid cancer in the US in 2008. Despite the increasing incidence of thyroid cancer, mortality rates have declined, leading to an estimate of 1,590 deaths from the disease in 2008.2 The opposite trends in incidence and mortality may be partially due to the fact that increased detection of small papillary cancers has significantly contributed to the overall incidence.3
Etiology
Approximately 75% of thyroid cancer cases are papillary thyroid carcinomas (PTC), while approximately 10% are follicular thyroid carcinomas (FTC). Both of these epithelial-derived cancers are considered to be differentiated thyroid carcinomas (DTC). Radiation therapy and ionizing radiation are well-documented risk factors for the development of PTC.4 Several studies have shown an increased risk for PTC in individuals who have Hashimotos’ thyroiditis, and recently a link with activation of the PI3k/Akt pathway has been suggested.5 Interestingly, despite increased incidence, prognosis may be better in individuals with underlying autoimmune thyroiditis.6 There also appears to be a familial component to the susceptibility to PTC.7 Many gene mutations associated with PTC, such as rearrangements of RET and NTRK1 tyrosine kinases and activating mutations of BRAF and RAS, ultimately activate the mitogen-activated protein kinase (MAPK) signaling cascade and thus promote cell division. BRAF mutations appear to be quite common in PTC, and were found in approximately 40% of cases in one study.8 The finding of different BRAF mutations within the various foci of multifocal PTC suggests that some foci arise independently from unrelated neoplastic clones.9 RAS mutations or PAX8-PPAR gamma 1 rearrangements are frequently seen in FTC.10 The prevalence of FTC may be increased in iodine-deficient areas compared with iodinesufficient regions.11 Higher serum thyroid-stimulating hormone (TSH) concentrations, even within the normal range, appear to be a risk factor for the development of DTC.12–14
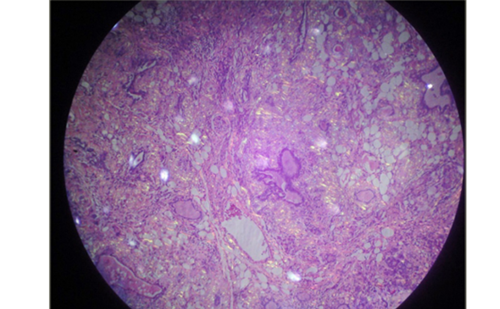
Presentation
DTC generally presents as a thyroid nodule and is diagnosed following a fine-needle aspiration. Such biopsies are approximately 95% accurate. There is a very small additional yield to repeating a fine-needle aspiration of a nodule initially diagnosed as benign. Out of 1,410 patients at one institution who had a repeat fine-needle aspiration of a nodule with a previous reading of benign cytology, 29 readings were changed to malignant or suspicious upon repeat aspiration.15 It is important to repeat non-diagnostic biopsies, generally with the aid of ultrasound guidance, as the malignancy rate in nodules with initially non-diagnostic cytology is around 5–8.5%.16,17 The examination of cytology specimens for mutations such as BRAF may ultimately become part of the diagnostic evaluation of individuals with PTC.10 Currently, there is no definitive test other than surgical excision for characterizing nodules deemed to be neoplastic follicular lesions.18 Galectin-3 expression has good specificity (93%) but relatively low sensitivity (78%) for predicting whether such lesions are malignant.19
Staging
Thyroid cancer staging systems attempt to organize patients into recognized groupings with similar prognostic indicators in order to assist with treatment selection and evaluation of response to therapy. However, the risks for death, disease recurrence, or disease progression in individual patients are not perfectly predicted by even the best-performing staging systems, resulting in limitations when a staging system is applied to individuals. Many staging systems have been proposed, including the tumor–node–metastasis (TNM)20 and the National Thyroid Cancer Treatment Cooperative Study (NTCTCS)21 (see Table 1) staging systems. These two systems categorize patients into four groups with successively worse prognosis with advancing stage. In both of these staging systems, age ≥45 years may advance a patient’s stage, reflecting the worse outcomes of older patients with DTC.22 Using the NTCTCS staging system 10-year product-limit overall survival was approximately 99, 92, 79, and 23% for stages I, II, III, and IV, respectively21,23 (see Figure 1). Gender is included as a criterion in one staging system,24 and appears to affect both outcomes25 and timeliness of presentation.26
Treatment
DTC cells generally retain some ability, albeit attenuated, to transport iodine,27 synthesize thyroglobulin, and respond to TSH.28 Despite their many biological differences, PTC and FTC are often treated similarly with thyroidectomy, possible radioactive iodine therapy with iodine-131, and the application of varying degrees of thyroid hormone suppression therapy.29,30 External-beam radiation and targeted therapy are generally reserved for patients who have macroscopic residual disease after surgical resection31 and progressive metastatic disease, respectively.30,32
Thyroidectomy
In the opinion of many experts, a total thyroidectomy is the appropriate operation once a diagnosis of DTC has been made.29,30 This is certainly the bias of the author. Complications are limited in the hands of an experienced surgeon,33 more sensitive surveillance is possible,34 and the risk for recurrent disease is lower.35 Intra-operative recurrent laryngeal nerve monitoring may be helpful in cases where the nerve is particularly at risk, although its role in routine thyroidectomy is not clear.36
Radioiodine Therapy with Iodine-131
A specific approach to thyroid cancer treatment is possible because of the presence of the sodium iodide symporter in thyroid follicular cells.27 However, there is less uptake of radioiodine in tumor tissue than in normal thyroid tissue.37 In addition, the half-life of radioactive iodine is shorter in malignant thyroid tissue than in benign tissue.38 As a result of these less favorable characteristics of tumor cells, iodine depletion39 and TSH elevation40 are employed to enhance sodium iodide symporter activity and attempt delivery of therapeutic doses of radioiodine to both thyroid remnants and tumor tissue41,42 Commonly used strategies are to engender an iodine-depleted state by means of a low iodine diet,43 and to increase ambient TSH levels by either withdrawing thyroid hormone or administering recombinant TSH.44,45 TSH levels typically rise to the goal level of 25–30mIU/l about three weeks after levothyroxine has been discontinued.46 Withdrawal protocols have typically been performed with the temporary use of triiodothyronine therapy. In theory this avoids a prolonged period of symptomatic hypothyroidism. However, a recent study did not confirm that the use of triiodothyronine in this manner reduced the symptoms of hypothyroidism.47
Radioiodine therapy can serve the dual purpose of ablating remnant thyroid tissue and treating residual or metastatic thyroid cancer.29,30,42 Empiric therapy involves the selection of radioiodine activity based on whether the intent is remnant ablation or disease treatment, taking into account sites of radioiodine uptake or known disease burden. As a general rule the lowest effective activity of radioiodine is recommended for remnant ablation,29 which may be in the 30–100mCi range. Higher activities are used for treatment depending on the extent of disease (see Table 2).30 Lymph node metastases may be treated with activities of 100–175mCi, unresected tumor penetrating the thyroid capsule may be treated with 150–200mCi, and distant metastases may be treated with activities of approximately 200mCi.
The use of recombinant TSH as preparation for remnant ablation has been shown to be effective in terms of both ablating thyroid remnants seen on radioiodine scanning and reducing serum thyroglobulin to undetectable levels.45 An advantage of a recombinant TSH protocol that was demonstrated in a recent trial was delivery of a significantly lower radiation dose to the blood.48 Presumably this was related to the greater renal clearance of radioiodine in the euthyroid state. In addition, disease recurrence rates after remnant ablation seem to be similar when preparation using recombinant TSH is compared with thyroid hormone withdrawal.49 Most studies have used an activity of 100mCi for recombinant TSH-assisted remnant ablation; however, 50mCi may be effective.50 Successful use of recombinant TSH to treat metastatic thyroid cancer has been reported,51 although careful selection of patients before use of this approach has been advised.52 One study showed less radioiodine uptake in metastatic lesions when recombinant TSH preparation was employed,53 which may necessitate the use of higher activities under such circumstances. An additional consideration, if a recombinant TSH protocol is chosen, is whether to dispense with a diagnostic whole-body scan in order to avoid two series of recombinant TSH injections. The omission of the diagnostic scan or the use of an intervening scan with iodine-123 are alternatives if the goal is remnant ablation. However, a pre-treatment diagnostic whole-body scan is critical when the treatment of metastases is being pursued.
Dosimetry is an alternative approach to selecting radioiodine activities.41,54 The procedure can be performed to determine the maximal activity of radioiodine that can be administered without causing excessive exposure of the bone marrow or whole body. This approach involves the dosimetric determination of the maximum tolerable activity. Lesional dosimetry seeks to define an activity that will deliver an adequate radiation dose to individual lesions.41 The advantage of dosimetry is that it avoids inadequate or excessive doses.54 Excessive doses may be a particular problem in the elderly.55 The disadvantage of dosimetry is that it is relatively time-consuming and not available in many institutions.
The principle of introducing therapeutic radiolabeled iodine into malignant cells has been extended to non-thyroid tumors. Attempts have been made to treat malignancies such as colon56 and breast57 cancer by introducing the sodium iodide symporter into their cells.
Thyroid Hormone Suppression Therapy
The suppression of serum TSH has been shown to be an important component of DTC management. A retrospective study showed that an undetectable TSH value was associated with longer relapse-free survival than higher TSH levels. TSH suppression was also an independent predictor of recurrence.58 A greater degree of TSH suppression tended to be associated with less disease progression in another cohort of high-risk patients,58 although the difference did not reach significance. A metaanalysis that quantified adverse clinical outcomes from 10 studies of TSH suppression therapy (including the two prior studies) also suggested a benefit of this approach.59
More recent data from a prospectively followed but non-randomized cohort of patients with thyroid cancer have shown improved overall survival with TSH suppression to undetectable and subnormal concentrations in those stratified as having high-risk and low-risk disease, respectively.23 Similarly, in a European cohort of patients with thyroid cancer, higher serum TSH levels were found to be associated with increased rates of thyroid-carcinoma-related death and relapse.60 Although the assumption has been that TSH suppression is effective by virtue of a reduced stimulus to proliferation associated with the lower TSH levels, it is also possible that there is an alternative mechanism. For example, triiodothyronine levels have been shown to be lower (in tandem with higher TSH concentrations) in individuals who are found to have DTC.14 Certainly, mutated forms of the triiodothyronine receptor that do not bind ligand are associated with mitotic abnormalities and induction of thyroid carcinoma in mouse models.61
External-beam Radiotherapy
This therapy is often able to achieve local control in individuals with disease that cannot be surgically resected. Radiotherapy is usually given following radioiodine administration, and seems to improve relapse-free survival specifically in the subset of patients with residual disease.31 Skin toxicity and mucositis are potential side effects, but these usually resolve after the therapy is complete. Radiotherapy can also be given to those requiring palliative treatment, including individuals with skeletal metastases.
Targeted Therapy
Traditional chemotherapy, such as doxorubicin, is generally ineffective for progressive thyroid cancer. Recently, several agents have been developed that capitalize on molecularly targeted treatment approaches instead of cytotoxic agents. One avenue of targeted treatment is to attempt to re-differentiate thyroid cancer cells that have lost the ability to take up radioiodine and thereby increase their expression of the sodium iodide symporter. Although this is a theoretically attractive approach, such agents have been associated with poor retention of radioiodine within cells in in vitro systems. Animal models have shown some success,62 but clinical experience has been somewhat disappointing.63 Agents currently in clinical trials include histone deacetylase inhibitors (depsipeptide and vorinostat) and DNA methylation inhibitors (decitabine).
A second approach is to employ multitargeted kinase inhibitors that interfere with the signal transduction pathways of thyroid cancer cells.32 The targets of these molecules include the RET tyrosine kinase, vascular epithelial growth factor (VEGF) receptors, BRAF kinase, and other membrane receptor kinases. Some agents also act as angiogenesis inhibitors. Examples of such agents are motesanib diphosphate, sorafenib, sunitinib, and axitinib. A phase II study of motesanib diphosphate showing some partial responses to treatment has recently been published.64 Other agents with potential include HSP-90 inhibitors, proteasome inhibitors, and COX-2 inhibitors.
Surveillance
Patients with DTC remain at risk for developing recurrent disease for as long as 20–30 years after their initial diagnosis, although recurrent or persistent disease is most frequently detected within the first two to five years.22,23,29,30 Thyroid cancer is unique in having a treatment modality that is also a means of disease detection. Thus, patients receiving treatment may be more likely to be documented as having disease, introducing a potential bias into studies of DTC outcomes.
The detection of recurrent DTC in those previously thought to be free of disease relies on several complementary modalities. These include basal or stimulated thyroglobulin measurements, stimulated whole-body radioiodine scans, and sensitive cervical ultrasonography. Whole-body scans appear to be the least sensitive tool for disease detection in low-risk patients.65 Together, recombinant TSH-stimulated thyroglobulin concentrations and cervical ultrasonography have a sensitivity of 96% and a specificity of 100% for detecting active disease.66 When measuring thyroglobulin concentrations it is critical to measure thyroglobulin antibodies simultaneously, as these antibodies invalidate the values obtained by most assays. A persistently elevated concentration of thyroglobulin antibodies seems to be associated with residual or recurrent disease.34 Furthermore, recurrence of disease is more frequently seen in patients with positive thyroglobulin antibodies compared with those without such antibodies.67 During follow-up testing, many patients who have stimulated thyroglobulin concentrations above 2ng/ml are eventually shown to have recurrent disease by other imaging modalities.68
Other imaging is also helpful for monitoring high-risk patients and following the disease burden in those with metastatic disease. Such imaging can include computed tomography (CT) scans, fluorodeoxyglucose positron emission tomography (FDG PET) scans, bone scans, and skeletal surveys.29,30
Optimal Management of Low-risk Patients
The optimal management of patients with low-risk thyroid cancer is a hotly debated topic. Total thyroidectomy is recommended for most patients.29,69 However, some experts advocate lobectomy for those without characteristics that may increase their risk such as, for example, tumors greater than 1–1.5cm, multifocality, regional metastases, or history of radiation exposure. Multifocality is quite common in PTC.22 Multifocality and tumor margins are characteristics that may not be evaluable until after a complete surgery. However, most of the controversy is centered on the issue of whether or nor radioiodine therapy is indicated.70 Even in the case of microcarcinomas, widely differing treatment approaches are taken, ranging from observation without surgery71 to almost universal application of radioiodine therapy following thyroidectomy.72 NTCTCS data support the use of radioiodine in low-risk patients with stage II disease, in whom this therapy is associated with prolonged overall survival.2373 Certainly, risks of therapy such as sialadenitis and early menopause may be of more relative importance in low-risk patients, in whom the benefits of therapy may be only modest. It is important for patients to understand these risks and benefits. The application of radioiodine therapy needs to be evaluated on an individual basis taking into account prognostic factors that may not be fully reflected in the patient’s stage, the importance of sensitive, unambiguous monitoring to the patient–physician team, and patient preference.
Aggressive TSH suppression does not appear to be warranted in low-risk patients. There was improved overall survival associated with a subnormal TSH in patients classified by the NTCTCS staging system as having stage II disease. Additional TSH suppression to yield an undetectable TSH did not further improve survival in these low-risk patients.23 Of interest, in this same analysis TSH suppression did not appear to be associated with improved outcomes in patients with stage I disease. Yearly physical examination and measurements of basal thyroglobulin level is the minimal standard of care for follow-up of low-risk patients. Periodic neck ultrasonography is generally also recommended for several years.29,30 Some experts are of the opinion that basal thyroglobulin measurements alone, when documented by a sensitive assay, are sufficient for following such patients.74 With respect to additional monitoring of low-risk patients, an undetectable thyroglobulin level following recombinant TSH administration provides reliable evidence for lack of disease recurrence. Very few cases of disease recurrence are identified by repeating measurement of recombinant TSHstimulated thyroglobulin measurements after a disease-free status has already been documented.75
Optimal Management of High-risk Patients
Total thyroidectomy and radioiodine therapy are both indicated for high-risk patients. Total thyroidectomy is associated with longer survival and fewer recurrences in such patients.23,35 Similarly, the use of radioiodine therapy is also associated with improved survival and decreased recurrence rates in high-risk patients.23,35,76 Data from a prospectively followed but non-randomized cohort of patients with thyroid cancer have shown improved overall and disease-specific survival with TSH suppression in those stratified as having high-risk disease.23 Furthermore, the suppression of TSH to an undetectable limit was associated with the greatest benefit. Other analyses confirm the benefit of TSH suppression as a management strategy.60
With respect to the follow-up of patients who have a high-risk category of disease or who have not been cured, it is very important to combine thyroglobulin measurements with imaging techniques that utilize diverse modalities. In addition to physical examination and basal thyroglobulin measurements, patients usually require cervical ultrasonography and diagnostic whole-body radioiodine scans. Cross-sectional imaging with CT or magnetic resonance imaging (MRI) and FDG-PET scanning may also be indicated. Such surveillance will not only help to assess the response to therapy, but will also guide the clinician in selecting additional therapy with radioiodine, surgery, or external-beam radiation. Patients who have stimulated thyroglobulin concentrations above 10ng/ml and an unidentified site of disease may benefit from empiric therapy with 100–200mCi.30,77 Such therapy may decrease disease burden, but does not appear to render patients disease-free. Furthermore, improved survival has not yet been demonstrated.30 Patients who have not responded to radioiodine, surgery, or external-beam radiation can be considered for clinical trials testing re-differentiation agents, multitargeted kinase inhibitors, or other novel therapies.32■