Thyroid cancer is the most common endocrine malignancy, being responsible for approximately 95 % of endocrine cases and 1.5 % of all cancers.1 Its incidence has increased substantially in recent decades and has been rising by 6.4 % per year over the past 10 years.1 This is due to a combination of an apparent increase resulting from more sensitive diagnostic procedures and of a true increase, a possible consequence of increased population exposure to radiation and to other still unrecognised carcinogens.2 In Europe there were approximately 52,
Thyroid cancer is the most common endocrine malignancy, being responsible for approximately 95 % of endocrine cases and 1.5 % of all cancers.1 Its incidence has increased substantially in recent decades and has been rising by 6.4 % per year over the past 10 years.1 This is due to a combination of an apparent increase resulting from more sensitive diagnostic procedures and of a true increase, a possible consequence of increased population exposure to radiation and to other still unrecognised carcinogens.2 In Europe there were approximately 52,900 new cases of thyroid cancer in 2012 (approximately 40,700 in women; 12,300 in men).3
Medullary thyroid cancer (MTC) is an uncommon type of thyroid cancer, representing around 4 % of thyroid cancers.4 It is also a challenging malignancy, since until recently surgery was the only effective therapeutic option. There is therefore a need for novel treatment options, especially for patients for whom surgery is unsuitable and with metastatic disease. This article aims to consider the current state of treatments, the efficacy and safety evidence from clinical trials supporting the tyrosine kinase inhibitors (TKIs) cabozantinib and vandetanib and their prospects for future use in this disease.
Prognosis, Clinical Presentation and Diagnosis
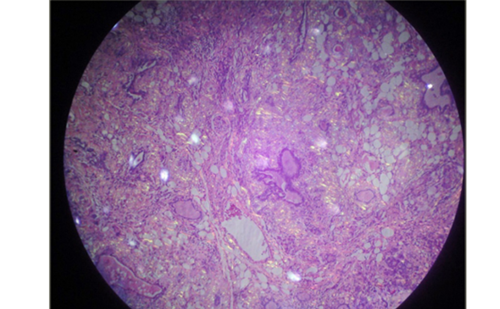
Thyroid cancers are classified into three groups. Differentiated thyroid carcinoma (DTC) represents 94 % of all thyroid cancers and includes three subtypes: papillary (80 %), follicular (11 %) and Hurthle cell carcinoma (3 %). Anaplastic (undifferentiated) thyroid carcinoma (ATC) represents 2 % of all thyroid cancers.4 And, as previously mentioned, MTC accounts for 4 % of the total cases.
MTC originates from the parafollicular C cells that produce calcitonin. MTC is generally more aggressive than follicular cell-derived thyroid cancer and is responsible for a large proportion of thyroid cancer-related mortality. The overall 5-year survival rate is 80–86 %, and the 10-year survival rate is 75 %.5,6 In patients with unresectable or metastatic MTC, the disease course is heterogeneous, ranging from disease progression during a period of months, to slowly progressing disease over many years. Patients with metastatic MTC have a poor prognosis, and they may experience symptoms such as pain from bone metastasis and diarrhoea. Progressive metastatic MTC is the main cause of medullary thyroid cancer-related morbidity and mortality; patients with distant metastases at diagnosis have only 40 % survival at 10 years.7
Although MTC is generally regarded as an indolent disease, patients with radiographic evidence of progressive MTC can have a substantial disease burden and high incidence of disease-related symptoms.8 Patients typically do not present with a characteristic pattern of symptoms but may report one or more of the following: a lump at the base of the neck, which may interfere with swallowing, hoarseness and diarrhoea.
Several diagnostic techniques for MTC are used routinely,9,10 among them thyroid fine-needle aspiration cytology (FNAC),11,12 although certain thyroid pathologies have similar cytology, making diagnosis difficult. The serum calcitonin level should also be measured: calcitonin is the main biochemical marker in MTC and can inform staging, postoperative management and prognosis.9,13 Calcitonin doubling time is an independent predictor of survival in MTC and may be superior to clinical staging.5,14,15 Carcinoembryonic antigen (CEA) is also a useful biomarker. In addition, CEA doubling time is a strong prognostic indicator for disease recurrence and death.14 If MTC is diagnosed or suspected on the basis of FNAC findings or calcitonin levels, ultrasonography should be undertaken to help confirm the diagnosis and to detect lymph node metastases.12,16 However, this often fails to locate metastatic disease and fluorine-labelled dihydroxyphenylalanine ((18)F-DOPA) or (18)F-FDG positron-emission tomography/computed tomography (PET/CT) may be used.17
Genetic testing is an important component of the diagnostic workup and is recommended in family members following a diagnosis of MTC.9,18 Up to 25 % of all MTCs are familial and carry a specific germline mutation in the REarranged during Transfection tyrosine kinase (RET) protooncogene.18 Even in apparently sporadic MTC the frequency of inherited disease ranges between 6.5–10 %.19,20 Molecular analyses show that approximately 55 % of MTC tumours have activating mutations in RET, including inherited and sporadic cases.21 These RET mutations in tumours, especially RET-M918T, have a strong negative prognostic impact. RET is targeted by most agents assessed in recent systemic therapy trials of MTC, along with vascular endothelial growth factor receptors (VEGFRs).21
Current Treatment Options for Medullary Thyroid Cancer
Treatment of MTC is based on evidence-based recommendations from the American Thyroid Association,9,22 although in practice different patterns exist in terms of diagnosis, treatment and long-term management.23 During the meeting of the European Thyroid Association [ETA] in 2009 some controversies arose.24 The most controversies were related to basal and stimulated serum calcitonin measurements, the extent of lymph node surgery, the extent of RET diagnosis and the management of inherited MTC.24
Surgical treatment of MTC is currently the only curative treatment modality and aims to provide local control of the cancer while maintaining laryngoesophageal function. Treatment involves total thyroidectomy, central neck dissection and autograft of an inferior parathyroid gland.25 Prophylactic surgery should be considered in inherited disease. Ipsilateral lateral neck dissection may also be performed if the primary tumour is >1 cm in size or there is evidence of positive nodes in the central neck. A contralateral lateral neck dissection may be considered in patients with bilateral tumours or extensive lateral adenopathy on the side of the primary tumour.26
Radiation therapy also plays a role in the treatment of MTC: external beam radiotherapy is an option for patients with locally advanced MTC to optimise locoregional control.26 Calcitonin and CEA are useful to monitor disease status after surgery; however, a minority of patients with nodal disease at the time of surgery have undetectable calcitonin levels postoperatively.25 Systemic chemotherapy and radiation therapy have limited benefit in disseminated MTC.27 There is variation among practitioners regarding when to initiate therapy in metastatic MTC. ETA guidelines are informative in this context.22
In 2009, a paradigm for targeted therapy in MTC was proposed following the discovery of genetic abnormalities in tumours, in particular mutations in the RET/PTC-RAS-RAF-mitogen-activated protein kinase (MAPK) axis and the phosphatidylinositol-3-kinase (PI3K)-protein kinase B (AKT)-mammalian target of rapamycin (mTOR) pathway.28,29 RET is the most studied of these potential therapeutic targets, and is able to activate a variety of signaling cascades, including MAPK and PI3K-AKT (see Figure 1).30
TKIs have been associated with limited or transient benefit arising from drug resistance.31,32 As a result, drug development has focused on agents capable of targeting several tyrosine kinases as well as other oncogenic pathways. Vandetanib (Caprelsa®, AstraZeneca) and cabozantinib (Cometriq®, Exelixis) are multitargeted TKIs with distinct but overlapping mechanisms of action that act to differing extents against multiple receptors including RET kinase, VEGFRs, epidermal growth factor receptor (EGFR) and the hepatocyte growth factor receptor MET.33 Both agents have been approved by the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA): cabozantinib was approved in the US in 2012 and in Europe in 2014; vandetanib was approved in the US in 2011 and in Europe in 2012.
Cabozantinib has been shown to inhibit the activity of receptor tyrosine kinases including MET, RET and VEGFR<2.34 In preclinical studies, cabozantinib showed significant antiangiogenic and antitumour activity in a broad range of tumour models, including a model of MTC with an activating RET mutation.35 It also resulted in decreased tumour invasiveness and decreased metastasis compared with agents targeting VEGF signalling without MET inhibition. Vandetanib also inhibits RET and VEGFR2, but in addition also targets EGFR.36,37
Vandetanib
Following evidence of antitumour activity in patients with hereditary MTC,38 and demonstration of durable partial objective responses and disease control in a phase II study,39 vandetanib was investigated in the Zactima Efficacy in Thyroid Cancer Assessment (ZETA) phase III clinical trial.40 This study randomised 331 patients with unresectable locally advanced or metastatic MTC (2:1) to vandetanib 300 mg/day or placebo. In the event of objective disease progression, patients could elect to receive openlabel vandetanib. At a median follow-up of 24 months the response rate (RR) was 45 % for vandetanib versus 13 % in placebo. (One per cent for placebo arm patients who had a response while on placebo, as opposed to after crossover to vandetanib). The median progression-free survival (PFS) was 19.3 months for placebo and this endpoint had not been reached for vandetanib at study completion, but a Weibull model indicated a predicted median of 30.5 months. The long PFS in placebo-treated patients reflects the inclusion criteria that did not require radiographic evidence of progressive disease within a specified time period prior to study entry; therefore, patients with slowly progressing disease could be included in the trial. However, patients were required to have a serum calcitonin level ≥500 pg/ml. The study met its primary objective of PFS prolongation with vandetanib versus placebo (hazard ratio [HR] 0.46; p<0.001). The improvement in PFS for vandetanib over placebo was also seen in all subgroups analysed including gender, race, World Health Organization (WHO) performance status ≥1 or =0, hereditary mutation, presence of metastatic cancer and prior therapy history. Overall survival data were immature at data cutoff (HR 0.89; 95 % confidence interval [CI] 0.48–1.65).
Common adverse events (AEs; any grade) occurred more frequently with vandetanib compared with placebo, including diarrhoea (56 % versus 26 %), rash (45 % versus 11 %), nausea (33 % versus 16 %), hypertension (32 % versus 5 %) and headache (26 % versus 9 %). The AE of most concern was corrected QT interval prolongation, a potential risk factor for torsades de pointes, particularly in view of the long terminal elimination half-life of the drug.
Cabozantinib
In a phase I study, (n=85, including 37 with MTC), 29 % of patients with MTC and measurable disease had a confirmed partial response. Overall, 49 % of the MTC patients with measurable disease experienced tumour shrinkage of 30 % or more. In addition, 41 % of the patients with MTC had stable disease for at least 6 months.41 Long-term disease control exceeding 2 years has now been demonstrated in these patients.42
Cabozantinib was subsequently investigated in the Efficacy of XL184 (Cabozantinib) in Advanced Medullary Thyroid Cancer (EXAM) phase III clinical trial.43 Following the vandetanib phase III trial, it was suggested that subsequent studies should include patients with more aggressive disease. This study therefore recruited 330 patients with unresectable locally advanced or metastatic MTC with radiographic disease progression per modified Response Evaluation Criteria in Solid Tumors (mRECIST) at screening compared with tumour measurements obtained within the previous 14 months. Patients were randomised 2:1 to receive cabozantinib (140 mg per day) or placebo. The estimated median PFS was 11.2 months for cabozantinib versus 4.0 months for placebo (HR 0.28; p<0.001) (See Figure 2). The short PFS in placebotreated patients reflected the inclusion criteria specifying only patients with radiographic evidence of progressive disease were eligible. The study found prolonged PFS with cabozantinib across all subgroups including by age, prior TKI treatment and RET mutation status (hereditary or sporadic). The RR was 28 % and responses were seen regardless of RET mutation status. Kaplan-Meier estimates of patients alive and progression free at 1 year were 47.3 % for cabozantinib and 7.2 % for placebo.
Subgroup analysis of the EXAM trial PFS data found that patients with mutations in genes encoding RET (pre-specified analysis) or RAS proteins (post-hoc analysis) experienced a significantly higher benefit than patients without those mutations.44 The RET status was determined in 65 % of the study participants; of these, 79 % had an activating mutation and 21 % were RET wild type. All RET mutation subgroups showed PFS benefit from cabozantinib treatment (although the confidence interval for the RET mutation-negative subgroup crossed 1.0), and demonstrated RRs between 22 % and 32 %. Patients harbouring a RET mutation had longer median PFS on cabozantinib (60 weeks) than patients with wild type RET (25 weeks; p=0.0001). The PFS benefit was slightly greater in patients with RET M918T, the most common RET mutation that is associated with poor prognosis45 (median of 61 weeks versus 36 weeks with another RET mutation; p=0.009). Patients with hereditary MTC had similar PFS to those with sporadic disease, and the presence of the common RET polymorphism G691S had no effect on either PFS or RR.
Since RAS gene mutations have been identified in some patients who lack a RET mutation, potential RAS gene mutations in the RET-wild type and RET status unknown arm were investigated and 16 patients were found to have a RAS gene mutation.44 Patients with a RAS gene mutation had a similar RR (31 %) and median PFS (47 weeks) to those with RET mutations (32 % and 60 weeks). The study concluded that the benefit observed in patients with an unknown RET mutation status might have been due to undetected RET or RAS gene mutations. Currently, the standard of care for MTC does not involve testing for these mutations in tumours.
Common cabozantinib-associated AEs included diarrhoea (63.1 % versus 33.0 %), palmar-plantar erythrodysesthesia (50.0 % versus 1.8 %), decreased weight (47.7 % versus 10.1 %), decreased appetite (45.8 % versus 15.6 %) nausea (43.0 % versus 21.1 %) and fatigue (40.7 % versus 28.4 %). Regarding to cardiac toxicity no clinically significant QT prolongation was observed in the trial. However, rare but potentially life-threatening AEs including gastrointestinal perforations, fistula development and haemorrhage were observed. Hypertension was reported in 32.7 % of patients with cabozantinib versus 4.6 % with placebo. AEs led to treatment discontinuation in 16 % of cabozantinibtreated patients and in 8 % of placebo-treated patients. The toxicity was considered significant but manageable.
Other Multikinase Inhibitors
Other promising multikinase inhibitors that have been investigated in MTC are summarised in Table 1 and include motesanib: a highly selective inhibitor of VEGFR, platelet-derived growth factor receptor (PDGFR) and KIT.46 Other kinase inhibitors include sunitinib47 and sorafenib,48,49 and axitinib.50 Lenvatinib, an oral multiple receptor tyrosine kinase (RTK) inhibitor targeting VEGFR-1 and -3, fibroblast growth factor receptor-1 and -4, RET, KIT and PDGFR, has received considerable attention as a promising therapeutic option,30,51 as has pazopanib.52 In preclinical studies, ponatinib has been shown to be a highly potent inhibitor of activated variants of RET found in MTC.53 Ongoing phase II trials in patients with MTC are investigating ponatinib,54 imatinib,55 nintedanib56 and anlotinib.57
Other Multikinase Inhibitors Other promising multikinase inhibitors that have been investigated in MTC are summarised in Table 1 and include motesanib: a highly selective inhibitor of VEGFR, platelet-derived growth factor receptor (PDGFR) and KIT.46 Other kinase inhibitors include sunitinib47 and sorafenib,48,49 and axitinib.50 Lenvatinib, an oral multiple receptor tyrosine kinase (RTK) inhibitor targeting VEGFR-1 and -3, fibroblast growth factor receptor-1 and -4, RET, KIT and PDGFR, has received considerable attention as a promising therapeutic option,30,51as has pazopanib.52 In preclinical studies, ponatinib has been shown to be a highly potent inhibitor of activated variants of RET found in MTC.53 Ongoing phase II trials in patients with MTC are investigating ponatinib,54 imatinib,55 nintedanib56 and anlotinib.57
Other Therapeutic Options
Expression of somatostatin receptor subtypes sst1, sst2 and/or sst5 have been shown in the majority (~80 %) of patients with MTC,58 leading to the investigation of somatostatin analogues in the treatment of MCTs. Pasireotide is currently being investigated alone and in combination with the mTOR inhibitor everolimus.59 Yeast-CEA (GI-6207), a therapeutic cancer vaccine genetically modified to express recombinant CEA, is also in early-stage clinical development.60 Radiopharmaceuticals are also available for the palliative treatment of advanced MTC: these include agents that target of the specific expression of receptors, such as 11In-octreotide, hormone transporters (radiolabelled meta- Iodobenzylguanidine [MIBG]) or molecular targets (radiolabelled anti-CEA monoclonal antibodies).61
Incorporating New Tyrosine Kinase Inhibitors into Current Treatment Paradigms
The availability of new targeted therapies requires a reconsideration of current treatment approaches for MTC. However, there is a need to identify a patient population most likely to benefit from these agents. These include patients with progressive distant metastases, patients without contraindications such as certain cardiac arrhythmias and patients in whom non-durable partial responses are expected to increase life expectancy. Patients with stable disease in whom the calcitonin or CEA doubling time are slow and those with multiple comorbidities may not be good candidates for multikinase inhibitors.
In terms of comparisons between vandetanib and cabozantinib, there are important differences in between the ZETA and EXAM trials (see Table 2). Among the inclusion criteria for EXAM trial was radiographic disease progression per mRECIST at screening compared with tumour measurements obtained within the previous 14 months, which was not an entry criterion in ZETA. The EXAM study population had rapidly progressive disease, reflected by a 4.0 month median PFS in the placebo group compared with 19.3 months median PFS for the placebo group in the ZETA trial. The EXAM study population also had advanced disease at baseline, reflected in the high level of baseline symptoms including pain and fatigue.43,62 To our knowledge, similar baseline data from the ZETA trial have not yet been published. In the EXAM trial, patients previously treated with TKIs (21 %) showed a significant benefit from cabozantinib, whereas the ZETA trial did not report data on previous TKI therapy. Both agents produced objective responses and both required dose reduction (35 % with vandetanib; 79 % with cabozantinib). The high percentage of dose reduction of the latter can be explained by the fact that the drug passed from phase I to stage III testing without a phase II trial. It is possible that a lower dose may be as effective, with improved tolerability and lower rates of dose reduction and/or discontinuation. The US Food and Drug Administration (FDA) has requested a postmarketing clinical trial to evaluate the safety and efficacy of a lower cabozantinib dose.63
Another important area for future study is the impact of cabozantinib in bone, one of the most common and early metastases seen in MTC.64 In a phase II study in advanced prostate cancer, cabozantinib had a substantial effect on disease in the bone, with an improvement in bone pain reported in 67 % of evaluable patients.65 Further clinical investigation is required to determine the effect of cabozantinib on bone metastases in patients with MTC.
Physicians treating patients with MTC now have a choice of two effective treatment options, but there are no data comparing these agents in the same study and patient population. For now, the choice of agent should be individualised.66 Cabozantinib might be preferred in patients with bone metastases, in those who are already receiving drugs to prolong the QT interval or who have significant electrolyte imbalances, although this needs further study. On the other hand, vandetanib seems to be better tolerated as dose reduction was required in only 35 % of patients in the ZETA study compared with 79 % receiving cabozantinib under the EXAM trial. However, the direct comparison of these drugs is necessary to confirm this hypothesis. Physicians should be familiar with the toxicity profiles of both drugs so that AEs relating to treatment can be identified at an early stage and prompt dose reductions can be implemented. Moreover, despite AEs related to drug toxicity, patients may complain of symptoms related to hormonally active metastases. The last ETA guidelines for metastatic MTC involved recommendation for these patients.22
It is important to remember that MTC is often an indolent condition, for which immediate therapy may not be required. There is a need to apply clinical judgement before initiating treatment. A calcitonin doubling-time of more than 2 years is a prognostic indicator of indolent disease and, in these patients, a ‘watch and wait’ strategy may be more appropriate.4 Conversely, symptomatic disease, where diarrhoea and pain are reported, can be a prompt to initiate therapy. There is a need to examine quality of life (QoL) measures in patients who are likely to be taking these therapies over a long period of time. There is also a need to investigate combined or sequenced therapeutic strategies. Monotherapy with vandetanib or cabozantinib affects only limited molecular targets and is unlikely to be curative because multiple signalling pathways and molecular mechanisms may be involved in disease progression. Combined approaches are likely to result in a broader range of AEs. However, since the toxicity associated with these agents has been reported as manageable, there is a rationale for investigating combined therapy and strategies for sequencing therapies.
In order to achieve clinical benefit and preserve QoL, it is important to identify patients who will benefit the most from these therapies. The role of RET and RAS gene mutations should be addressed in future studies of cabozantinib and vandetanib.67 The extent of benefit may depend in part on RET genotype.68 Both the EXAM and ZETA studies showed a PFS advantage in patients with RET mutation-positive tumours, including patients with the poor-prognosis mutation M918T.40,43,68
Summary and Concluding Remarks
There is a lack of effective therapy for patients with MTC, for which survival is currently worse than in differentiated thyroid cancer, and new treatment options are urgently needed. The multikinase inhibitors represent a paradigm shift in the treatment of MTC and have achieved prolonged responses and improved PFS. Vandetanib and cabozantinib have been approved for the treatment of advanced MTC, with several other agents in clinical development. However, MTC can be a slowgrowing disease and there remains a need for long-term data to determine the benefits of these agents in terms of overall survival and QoL. There is a need for updated guidelines related to the treatment of advanced MTC.
It is likely that the number of treatment options for this patient population will continue to grow, but there are at present limited data to inform choices of which drug should be used first. There is a need to define the patient population at risk so that patients with indolent disease are not exposed to toxic agents prematurely when survival is not affected. In conclusion, multikinase inhibitors represent a significant landmark in the treatment of MTC.