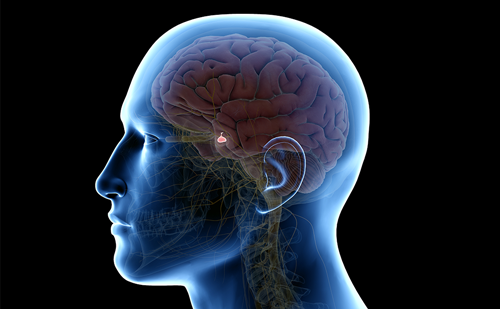
Prolactin (PRL) is a single-chain peptide hormone secreted from lactotroph cells of the anterior pituitary. The main physiological role of PRL is to promote milk secretion after childbirth.1 PRL secretion is tonically inhibited by dopamine (DA) from neurons in the hypothalamus.
Physiology and Pathophysiology of Hyperprolactinaemia
Prolactin (PRL) is a single-chain peptide hormone secreted from lactotroph cells of the anterior pituitary. The main physiological role of PRL is to promote milk secretion after childbirth.1 PRL secretion is tonically inhibited by dopamine (DA) from neurons in the hypothalamus.
Physiology and Pathophysiology of Hyperprolactinaemia
Since the early 1970s, it has been possible to measure PRL in human blood in clinical practice.2 Hyperprolactinaemia can be defined as abnormally high levels of PRL in blood – in women above 25μg/litre, in men above 15μg/litre. It occurs as a physiological condition in females who are pregnant or lactating. Pathological hyperprolactinaemia is a common finding in clinical endocrinology, often leading to reproductive and sexual dysfunction. In women, the most frequent symptoms are amenorrhoea, galactorrhoea and infertility.3,4
Pathological hyperprolactinaemia has several possible causes. It is important to diagnose these different possible causes of hyperprolactinaemia as pituitary disorders (pituitary tumours, inflammatory and infiltrative diseases and hypothalamic stalk interruption) or hypothalamic disorders, such as hypothyroidism, medications that alter the inhibitory actions of DA (antipsychotics, antiemetics, antihypertensives, tricyclic antidepressants, opiates and protease inhibitors), reduced PRL elimination (renal failure) and abnormal molecules (macroprolactinaemia).
However, a major objective in a patient with hyperprolactinaemia is to identify a PRL-producing pituitary adenoma and differentiate it from secondary hyperprolactinaemia due to a tumour compressing the pituitary stalk, as the therapy will differ.5
Treatment of PRL-producing Tumours in Women
In women, the majority of the PRL-secreting tumours are small at the time of diagnosis. Therefore, symptoms due to local mass effect, such as headache, visual field defects and hypopituitarism, are uncommon.3,6 Medical therapy with DA agonists is effective at inhibiting and normalising PRL levels, restoring gonadal function and reducing tumour size.7–9 Thus, DA agonists are the treatment of choice in most patients with hyperprolactinaemia. Surgery is recommended in patients intolerant or resistant to DA agonists.10–13
However, surgery has also been proposed as the therapy of choice in patients with micro-adenomas.10,14 In addition, according to some studies, the majority of untreated microadenomas do not progress into macroadenomas.15–17 The results of different treatment modalities in women with prolactinomas can now be evaluated for a period of up to 30 years.
Medically Treated Patients
Normalisation of PRL levels was achieved in 71% of women studied for up to three decades.18 Eighty per cent of these women showed complete or partial reduction in their micro- or macroadenoma, 17% had a stable tumour and 3% had an increase in tumour size due to non-compliance or side effects of the DA agonist (bromocriptine). All macroadenomas showed complete disappearance or partial reduction of the tumour mass.
Surgically Treated Patients
The surgically treated women in a long-term study were all operated on with the transsphenoidal technique. A few patients underwent surgery as primary treatment due to the practice during earlier years, but most women were operated on because of side effects or lack of response to medical treatment. Fifty-three per cent were cured at follow-up, i.e. PRL levels were normalised without treatment. However, 77% exhibited no detectable tumour at follow-up. Partial pituitary insufficiency or panhypopituitarism occurred in a few patients.18 Other studies evaluating surgical intervention by the transsphenoidal route reveal a success rate of approximately 75% for microprolactinomas, while the corresponding success rate for removal of a macroprolactinoma was only approximately 25% in the long term, the limited results partly depending on a high frequency of recurrence.19 Except for pituitary deficiency, complications associated with surgical resection of a prolactinoma, such as meningitis, bleeding and diabetes insipidus, should also be considered.
Radiotherapy
Conventional radiotherapy has been observed to decrease tumour size and PRL secretion, but hypopituitarism is often induced so this treatment only tends to be considered when both pharmacotherapy and surgery fails.20 More modern Gamma Knife radiosurgery has been given to a limited number of patients with long-term follow-up.18 These patients showed normalised PRL levels in approximately 50% with adenoma disappearance or decreased tumour size at follow-up in all cases and no signs of hypopituitarism.
Clinical Perspectives
It has been demonstrated that there is a correlation between pre-treatment PRL levels and tumour size.14,21,22 In general, macroprolactinomas are typically associated with PRL levels over 250μg/litre.12,13 In rare cases, a macroprolactinoma with PRL levels around 100μg/litre may be explained by a low PRL secretion rate.18 However, since hyperprolactinaemia not exceeding 100μg/litre is, in the vast majority of prolactinomas, related to a microadenoma, macroadenomas with PRL <100μg/litre must be very carefully evaluated as they are likely to be clinically inactive tumours or multiple hormone-secreting adenomas. This is of great importance with respect to therapy, because the treatment of a non-secreting adenoma or multiple-hormone-secreting adenoma is surgery.
Observational studies of women with hyperprolactinaemia and PRL-producing tumours clearly show that medical therapy is effective in most patients after short-term treatment as well as in the long term – up to three decades. In the majority of patients, PRL levels normalise, the tumour size decreases and, in some cases, the visible tumour mass disappears. Normal ovarian function is restored in most women, which is of great importance due to the low mean age at diagnosis, approximately 30 years.
Three different DA agonists are now commonly used in the treatment of hyperprolactinaemia – bromocriptine, cabergoline and quinagolide. Due to the fact that bromocriptine was the only DA agonist available for many years, all patients on long-term follow-up with medical treatment have used this drug. However, several studies in patients with prolactinomas have demonstrated that both cabergoline and quinagolide are at least as effective as, or superior to, bromocriptine in normalising PRL levels and reducing tumour size and is also significantly better tolerated.23–29
Surgery in patients with prolactinomas shows a long-term cure rate just over 50% in several studies, including both micro- and macroadenomas.14,18,30 The outcome after surgery is much better in microadenomas, with a cure rate of approximately 75%. However, with the risk of relapse after surgery, and in view of the effectiveness of medical treatment, DA agonists ought to be the first-line therapy for prolactinomas.
The limited experience of Gamma Knife radiosurgery in the treatment of prolactinomas shows that this therapy should be further evaluated. Indications for radiosurgery – for instance intolerance to DA agonists or DA resistance of the tumour – should be analysed. In addition, the long-term side effects of radiosurgery, particularly a possible increase in pituitary insufficiency, must be studied.
Conclusions
Hyperprolactinaemia is a common disorder and prolactinomas, especially microprolactinomas, are a frequent finding in young women. Medical treatment with DA agonists are effective in correcting hypogonadism, normalising PRL levels and reducing tumour size in most patients after short-term therapy. Even after long-standing disease up to 30 years, the majority of women are effectively treated with DA agonists. However, the possibility of transsphenoidal surgery must be considered in some cases.
The future role of Gamma Knife surgery in the treatment of prolactinomas should be evaluated. ■