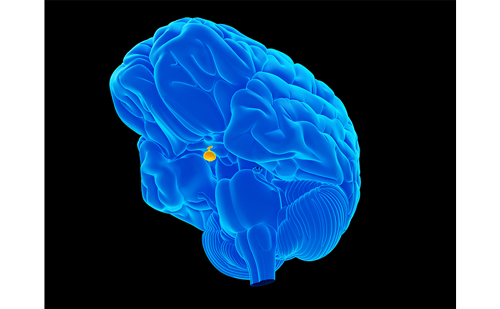
Growth hormone (GH) is a polypeptide hormone consisting of 191 amino acids, synthesised, stored and secreted by somatotroph cells in the lateral wings of the anterior pituitary, in a gender- and age-dependent manner.
GH acts to mediate widespread effects, controlling growth and metabolic functions, playing a role in maintaining the integrity of many tissues. GH continues to be secreted in adult life after growth cessation, influencing fuel metabolism, body composition, physical performance and psychological function.
Growth hormone (GH) is a polypeptide hormone consisting of 191 amino acids, synthesised, stored and secreted by somatotroph cells in the lateral wings of the anterior pituitary, in a gender- and age-dependent manner.
GH acts to mediate widespread effects, controlling growth and metabolic functions, playing a role in maintaining the integrity of many tissues. GH continues to be secreted in adult life after growth cessation, influencing fuel metabolism, body composition, physical performance and psychological function.
GH deficiency (GHD) can manifest in childhood as growth failure, delayed bone age and slow growth velocity, while in adults the picture is more complex and is characterised by negative effects on body composition, cardiovascular functions and poor quality of life. Life expectancy is reduced in adult patients with GHD as a consequence of cardiovascular and cerebrovascular events. Most, if not all, of the abnormalities improve or normalise with GH replacement. Side effects are minor and can be minimised by individualising dosage requirements.
Epidemiology and Etiology
In the UK the incidence of GHD in children has been estimated at around 1:60,000, while in the US approximately 1:3480. A Swedish survey reports the prevalence of GHD in adults 175 cases per million.
GHD in both children and adults is more frequently caused by pituitary and peripituitary tumours, and neurosurgery for their treatment is a common cause of GHD. It may be also secondary to destructive lesions such as trauma, irradiation or infiltrative diseases; recently, genetic abnormalities have been demonstrated to cause GHD and more complex pituitary disorders, especially in children. It has been reported that 1% of cases is determined by an autoimmune aggression to the pituitary cells; however, several cases of GHD remain of unknown etiology and childhood-onset GHD is most commonly considered idiopathic. On the other hand, thanks to the recent advances in the understanding the physiology of pituitary and in the amelioration of diagnostic procedures, many cases previously thought idiopathic are now classified among the autoimmune or genetic forms of GHD.
Autoimmune GHD
An autoimmune involvement has been recognised in most endocrine diseases previously considered to be idiopathic. Since 1957, Witebsky et al. have established criteria, subsequently revised by Rose and Bona in 1993, to define autoimmune diseases. On the basis of these criteria, many diseases are now included in this category. Concerning this, some forms of GHD can fall in the group of autoimmune entities; to this regard, Goudie and Pinkerton described the first case of lymphocytic hypophysitis (LYH) and proposed that autoimmunity could play a role in affecting the pituitary gland. They described the occurrence of anterior hypophysitis and Hashimoto’s disease in a young woman who presented with post-partum amenorrhea and hypothyroidism. Since its first description, several cases have been described and its frequency has increased with time. LYH classically presents as a pituitary mass in young women in late pregnancy or early post partum. LYH is frequently associated with other autoimmune diseases and it is possible the detection of other organ and non-organ-specific autoantibodies configuring in some cases an autoimmune polyendocrine syndrome (APS). It usually causes adrenocorticotropic hormone (ACTH) deficiency, in isolation or in association with thyroid stimulating hormone (TSH) deficiency. These defects are considered the direct result of the autoimmune attack on the pituitary cells. GHD during LYH is reported with a variable prevalence between the various studies. It does not seem to be frequent, however, GH function has not always investigated in all patients; so the true prevalence may be underestimated.
Auto-antibodies are the hallmark of autoimmunity. Auto-immune GHD can be suspected in the presence of antipituitary antibodies (APAS) and when other causes of GHD can be excluded. Antibodies to GH-secreting cells were first described by Bottazzo et al. in a girl with Turner’s syndrome, GH deficiency and a familial history of autoimmune polyendocrinopathy. Subsequently, these antibodies were detected in three out of 397 children with growth failure and in one out of four patients with idiopathic GH deficiency.
By the immunoblotting method, Crock et al. showed the presence of antibodies against a 43-45kDa membrane protein in one of 19 idiopathic GH-deficient children, but in none of normal controls. Subsequently, the same authors found that antibodies against a 49kDa pituitary cytosolic protein were present in 70% of patients with biopsy-proven LYH and 55% of patients with suspected hypophysitis, including patients with isolated ACTH deficiency or patients with GHD associated to disorders of the secretion of other pituitary hormones and with other autoimmune diseases. However, aminopeptidase A (APA) reactive to this protein were found also in many patients with other autoimmune endocrine diseases without GHD or LYH and in 20% of patients with hypopituitarism secondary to pituitary adenomas. Recently, the same author identified the 49kDa pituitary cytoplasmatic protein as an α-enolase, an enzyme ubiquitously expressed. Antibodies to α-enolase are not specific for LYH because they are frequently present in other autoimmune diseases. However, these authors suggested that these antibodies may be helpful in the diagnosis of patients with LYH who would otherwise need pituitary biopsy.
A recent study by Nishiki et al. demonstrated GHD in nine out of 25 patients (36%) with biopsy-proven or clinically-suspected hypophysitis; GHD was associated with multiple pituitary hormone deficiencies. Three showed serum antibodies against 68, 49 and 43kDa human pituitary membrane antigens, the magnetic resonance imaging (MRI) showed an intrasellar mass with gadolinium enhancement.
By radioligand, some authors detected antibodies against human GH and against two novel pituitary proteins, namely PGSF1 and PGSF2 (pituitary gland-specific factor) in patients with LYH, suspected on the basis of characteristics on MRI. No relation between anti-GH antibodies and serum GH concentrations were found in this study; however it is not clear whether patients in this study had GHD.
APA against a 22kDa protein (GH) were identified in seven patients with GHD and their levels significantly decreased after GH replacement therapy. Instead, other failed to find a correlation between anti-pituitary hormone antibodies and hormonal deficiencies, because anti-GH antibodies were also present in patients with pituitary adenomas, so these antibodies were not considered specific for endocrine deficiencies by the authors. However, we suppose that other than anti-pituitary hormone antibodies are involved in GHD; to this purpose, we performed an evaluation of APA, by indirect immunofluorescence in adults with idiopathic GHD (IGHD), or with pituitary adenoma and in patients with autoimmune endocrine diseases. APA were found at high titres in 33% of patients with IGHD but in none of patients with acquired GHD. We did not observe diminution of immunostaining when sera of APA-positive patients were pre-adsorbed with GH: this finding seems to exclude the possibility that apa were directed against GH. APA were also detected at low titres in six of 20 patients (30%) with pituitary adenomas and in 40 of 180 (22.2%) patients with autoimmune endocrine diseases; 35 of them at low titres (87.5%) and five at high titres (12.5%). APA positive patients at low titres had normal pituitary function, whereas all APA-positive patients at high titres) had a severe isolated GHD. On the basis of these results, we suggested that immunofluorescence is a good approach for the detection of APA. In particular, APA (only when present at high titres) may be considered a good marker of pituitary involvement, not only in patients with apparently isolated idiopathic GH deficiency but also in adults with autoimmune endocrine diseases with selective GHD. Retesting the APA positive sera of same patients previously studied by a four-layer double indirect immunofluorescence we were able to demonstrate that the somatrophs are the target of APA in patients with IGHD, while in patients with GHD associated with other autoimmune diseases, APA were directed not only against GH-, but also to other pituitary hormone-secreting cells.
Data about GHD and LYH in children are lacking in literature; apart from the initial description by Bottazzo et al., GHD secondary to LYH has been described in a girl with severe autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy (APECED), and presenting with antipituitary antibodies reactive to a 43-45kDa membrane protein and a perihypophyseal ‘halo effect’ with gadolinium enhancement on magnetic resonance imaging (MRI), suggestive of hypophysitis. Another case of GHD in a girl with APECED has also been described; in this case the radiological finding was empty sella.
Recently, we evaluated the presence of APA in prepubertal children with idiopathic GHD to identify in possible APA-positive children with GHD whether somatotrophs or other pituitary hormone-producing cells are targeted by these antibodies. Starting from 2002, we studied IGF-I levels, GH secretion under two stimuli and APA in 26 children with IGHD, 33 children with GHD due to other hypothalamus or pituitary lesions and 40 normal controls. We found APA immunostaining GH-secreting cells in seven out of 26 IGHD children, but in none of those with other hypothalamus or pituitary lesions. Thus, we concluded that several cases of apparentely idiopathic GHD in children could be caused by an autoimmune aggression to pituitary gland which can be revealed by detection of APA at high titre immunostaining GH-secreting cells.
In keeping with the observation that GHD can be caused by autoimmune events not only in adults, but also in children, Iughetti et al. searched for APA in some coeliac children who did not show the expected catch-up growth after 12 months of gluten-free diet (GFD). They were tested for GH secretion by two stimuli and APA were evaluated in our laboratory. Five out of the seven patients showed an impaired GH response to the stimuli and all but one resulted positive for APA at high titre. These results suggest that the lack of catch-up growth in children with coeliac disease (CD) submitted to GFD may be due to autoimmune GHD and that the prevalence of LYH in children is probably more elevated than that so far considered. The detection of APA in children with CD whose growth velocity does not improve during GFD can help to identify those with autoimmune GHD, thus allowing an appropriate treatment, if any.
Conclusion
Notwithstanding the numerous studies, the immune reaction against pituitary cells during LYH and in particular GHD still awaits confirmation from a qualitative and quantitative point of view. The differences in the methodologies employed, in the substrate used for the detection of antibodies, the lack of standardisation of the detection techniques that interferes with interlaboratory comparisons, the selection of patients and the not complete evaluation of pituitary function in all patients could explain the discrepancies between the various reports.
The lack of animal models of experimental LYH, reproducing the full picture of the human disease, due to the resistance of pituitary to the induction of the disease, limits the comprehension of the mechanisms underlying GHD and LYH.
On the other hand, the relevant target autoantigens in GHD and LYH have not yet been identified; their future identification may help in the elucidation of the events leading to the development of the disease.
In this connection, an investigation of the correlation between APA, hormonal and hystopathological findings in a large cohort of patients with biopsy-proven LYH is still desiderable.
MRI can help in diagnosing LYH, but pituitary biopsy remains the diagnostic gold standard. However, since pituitary biopsy cannot always be feasible and MRI characteristics often overlap with those of adenoma, a serological marker helping in diagnosis of autoimmune GHD is required, avoiding the need for neurosurgery with its attendant risk. In this connection, we advise the detection of APA by immunofluorescence, in at risk subjects as a useful tool that may contribute to the diagnosis, especially when pituitary biopsy cannot be performed and/or when MRI is not conclusive. ■
A version of this article containing references can be found in the Reference Section on the website supporting this briefing (www.touchbriefings.com).