Prolactin (PRL) is a 199-amino-acid polypeptide with molecular weight of 23 kilo Daltons (kDa) secreted by lactotroph cells of the anterior pituitary that plays a pivotal role in a variety of reproductive functions.
Prolactin (PRL) is a 199-amino-acid polypeptide with molecular weight of 23 kilo Daltons (kDa) secreted by lactotroph cells of the anterior pituitary that plays a pivotal role in a variety of reproductive functions. Besides this 23kDa PRL (little PRL), constituting generally 85-95% of circulating PRL, there are two other forms of this hormone in the circulation, namely dimeric or big PRL (45–50kDa) and macroprolactin (big-big PRL, 150–170kDa).1,2 Prolactin secretion is under hypothalamic regulation, with dopamine acting as predominant inhibitory factor (via activation of D2 receptors on lactotrophs), and TRH and VIP as stimulatory factors.1,2 Several other factors has been suggested to be involved in regulation of PRL secretion but there is no final proof of their significance.1,3-5
Hyperprolactinaemia, i.e. an excess of PRL above a reference laboratory’s upper limits (in women 20μg/L, in men 15μg/L), is the most common endocrine disorder of the hypothalamic-pituitary axis. It occurs in some physiological conditions, such as pregnancy and lactation.6,7 Short-term rise in PRL concentrations can be induced by stress, sleep, physical effort, hypoglycemia1,2,8 and also is a part of human sexual response (orgasm).9 Pathological hyperprolactinaemia has several possible causes.
Etiology and Pathogenesis
Hyperprolactinemia can be caused either by organic lesions within the hypothalamic-pituitary axis or by functional disturbances of hypothalamic regulation of PRL secretion. The most frequent cause of the organic hyperprolactinaemia is the prolactinoma – a pituitary adenoma derived from pituitary lactotrophs and excessively secreting PRL. Prolactinoma is also the most frequent type of pituitary adenoma (30–50%). As with the other pituitary adenomas, the formation of prolactinoma results from the mutation of a single glandular cell (tumor initiation) followed by a subsequent mutation and/or by functional disturbances favouring the tumour growth (tumour promotion and progression). At the time of diagnosis, prolactinoma may have different sizes and belongs to either microadenomas (diameter < 1cm) or to macroadenomas (diameter > 1cm). The tumour size is usually correlated with serum PRL levels.7 In particular patients, prolactinomas may differ in their aggressiveness. Tumours in men are considered to be more aggressive than those in women.10 However, the malignant prolactinomas (PRL-secreting pituitary cancers) are very rare and can be diagnosed only in the presence of distant metastases within the central nervous system or at the periphery.11
Apart from prolactinomas, organic hyperprolactinaemia may be caused by other types of pituitary adenoma that co-secrete PRL. The co-secretion of PRL is observed mostly in GH-secreting pituitary adenomas in patients suffering from acromegaly.7 Last but not least, organic hyperprolactinaemia may be produced by other organic lesions of hypothalamus including the pituitary stalk (inflammatory lesions, tumours, empty sella syndrome), when these lesions destroy hypothalamic dopaminergic neurons or disrupt the hypothalamic-pituitary connections. The mechanism of hyperprolactinaemia in such cases is connected with failure of the negative control of PRL secretion by hypothalamic dopamine.7
Hyperprolactinaemia may also occur in cases when the excessive PRL production is not connected with detectable lesion within the hypothalamic-pituitary system. The iatrogenic hyperprolactinaemia may be caused by the intake of drugs enhancing PRL secretion. The list of these drugs includes: dopamine receptor blockers (e.g. antipsychotic drugs: haloperidol, chlorpromazine, perphenazine, and antimimetic or gastric motility regulators: meto-clopramid, domperidone), antihypertensive drugs (e.g. reserpine, alpha-methyl-DOPA, vera-pramil), antidepressants (fluoxetine, imipramines), H2 antagonists (ranitidine, cimetidine), estrogens (at high doses), opiates, protease inhibitors (zidovuline, ritonavir, indinavir), and GnRH agonists (triptarelin).7,12 Hyperprolactinaemia may also accompany the primary hypothyroidism, chronic renal failure, liver cirrhosis, adrenal insufficiency and polycystic ovary syndrome.6,7,13,14
The idiopathic hyperprolactinaemia is diagnosed in cases of PRL hypersecretion when any detectable causes of PRL excess cannot be indicated. However, the presence of a very small, undetectable microprolactinoma cannot be excluded in such cases. On the other hand, because of a relatively high frequency of the incidental non-functional pituitary microadenomas in the population (4-20%), the detection of a microadenoma in the MRI does not exclude the idiopathic hyperprolactinaemia.15
Symptoms
There are several symptoms of hyperprolactinaemia which can be divided into two main categories, the first depending on direct effect of PRL excess and the second being a consequence of the resulting hypogonadism.
In women, clinical presentation of hyperprolactinaemia includes amenorrhea or oligomenorrhea (depending on the degree of PRL excess) occurring in over 95% cases, infertility, decreased libido, galactorrhea, hypogonadism (its degree generally is proportional to the degree of PRL excess) with related osteopenia and increased body weight.6,7,13,14
In men, hyperprolactinaemia is associated with infertility (due to oligospermia and diminished ejaculate volume), gynecomastia (rarely with galactorrhea), impaired libido and impotence (unresponsive to testosterone treatment and associated with decreased muscle mass, body hair, and osteoporosis).6,7,13,14,16
Diagnosis
Initial diagnosis of hyperprolactinaemia is based on repeated findings of the elevated PRL serum levels. Then, physiological, drug-induced and other secondary causes of PRL excess should be excluded. According to our experience, the estimation of circadian PRL profile (see Figure 1) is more reliable than the morning measurement. The controversial results of pharmacological tests used in the past two decades, together with the availability of MRI, practically excluded these tests in the work-up of hyperprolactinaemia.17
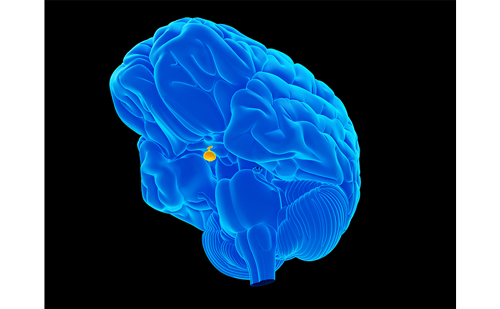
Generally, PRL concentrations between 25 and 200μg/mL may be characteristic of any cause of hyperprolactinaemia, whereas its level exceeding 200μg/mL (especially with disturbed circadian changes) usually indicates the presence of prolactinoma. Lower elevations of PRL concentrations (usually below 150ug/L) along with the presence of macroadenoma in MRI, suggest either a pituitary tumor co-secreting PRL or a tumor non-secreting PRL but inducing hyperprolactinaemia by destruction of dopaminergic hypothalamic neurons. Pituitary imaging, preferably MRI, should be performed to establish whether PRL-secreting tumor (micro- or macroprolactinoma; Figure 2) or other lesions (e.g. neoplastic or inflammatory lesions, empty sella syndrome) in the pituitary region or hypothalamus are present.7,14 When PRL-secreting pituitary tumor is diagnosed, it is recommended to test other pituitary hormones, especially to measure GH or IGF-I, because the existence of mixed PRL- and GH-secreting adenomas is quite common.
Macroprolactinaemia
In the beginning of the 1980s, there were two cases of hyperprolactinaemia in which despite high PRL levels, clinical symptoms of the disease were lacking and maintained fertility were described. In these cases, circulating serum PRL was predominantly in the form of large complexes (big–big PRL, macroprolactin).18 In 1985 Jackson et al.19 first introduced the term ‘macroprolactinaemia’ for such form of hyperprolactinaemia. The term ‘macro prolactin’ is used for large (more than 150kDa) immunocomplexes of PRL with immunoglobulin G (IgG), or rarely for aggregates of monomeric PRL molecules.2,20,21 It is estimated that macroprolactin may be responsible for elevated PRL concentrations in 10–26% of patients with idiopathic hyperprolactinaemia.21
Although majority of patients with macroprolactinemia do not have any significant clinical symptoms, especially considering reproductive dysfunction, some of them occasionally present such symptoms as oligomenorrhrea or minimal galactorrhea. Also pituitary imaging (by CT or MRI) is generally negative in macroprolactinemic patients.21,22
Since macroprolactinemia can be recognized by a simple polyethylene glycol method (PEG) it is reasonable to test a possible macroprolactin presence in hyperprolactinemic patients, especially in those with idiopathic hyperprolactinaemia and/or in individuals with the lack and/or poorly marked symptoms.
Treatment
The treatment of hyperprolactinaemia includes medical therapy or surgical therapy. The objectives of the therapy is to lower PRL levels, and as a consequence to restore normal gonadal function, including restoration of fertility. In the case of prolactinoma, additionally a reduction (or removal) of tumor mass and correction of visual or neurological abnormalities should be achieved. No specific treatment (only periodic observation) seems to be required when hyperprolactinaemia is asymptomatic.14
Medical Therapy
The first-line therapy of hyperprolactinaemia is treatment with dopamine agonists with proven efficacy in lowering PRL levels and restoring reproductive function. Among dopamine agonists, bromocriptine, carbegoline, and quinagolide are the most frequently used.
Bromocriptine was developed in the 1970s and, therefore, has the longest track record. In most cases it is effective at a typical dose of 2.5–5.0mg/d.7,14 However, short half-life (3.3 h) and duration of the action for 8-12 hrs as well as common side effects (including high frequency of gastrointestinal upset, sedation, and hypotension) requiring withdrawal of bromocriptine in almost 12% of patients,23 limits to some extent its use.24
Cabergoline (D2 receptor specific agonist) is currently most widely used in the treatment of hyperprolactinaemia because of its half-life of 65 hours, longer duration of action (7–14 days), greater potency, and low frequency of side effects (withdrawal in only 3.2% of patients23). A typical dose of cabergoline is 0.5–1.0 mg/wk.7,14,24
Quinagolide is another D2 receptor-specific agonist introduced in the therapy of hyperprolactinaemia (typical dose – 0.075mg/d). It is an agent with a quick and simple titration, with significantly less frequent and intense side effects, and therefore, better-tolerated than bromocriptine.7,24
Summarising, treatment with the dopamine agonists is very effective in most cases of hyperprolactinaemia. It may be beneficial in all causes of the disease, including micro- and macroprolactinoma. Normalization of PRL levels, restoration of gonadal function, and reduction of tumor size (or even its disappearance) was observed in over 70% of patients.25 The duration of the therapy should be individualised, although some authors have suggested the lowering of dopamine agonists dose after two to three years of normal PRL concentrations, and stopping the therapy if the PRL levels remain unchanged after one year at reduced dose.14 Of course, regular monitoring of the patient is necessary after complete discontinuation of the therapy. In hyperprolactinaemia caused by hypothyroidism, renal failure, liver cirrhosis, polycystic ovary syndrome, or drugs use treatment should concentrate on basic disease.
Surgical Therapy
Is it very high effectiveness of medical therapy with dopamine agonists, there is a significant reduction in the necessity of surgical therapy. Although surgical therapy is as effective as medical therapy, and seems to be more cost-effective in the long term,26 the decision to perform surgery becomes now a little bit controversial, especially as a first-choice therapy. It seems currently that surgical therapy should be restricted to patients intolerant or resistant to dopamine agonists, and to those with nonfunctional pituitary adenomas or other nonlactothroph adenomas associated with hyperprolactinaemia.7,14,27
Conclusions and Perspectives
It should be stressed that the finding of elevated PRL serum concentrations constitute the beginning of diagnostic procedure and, after exclusion of physiologic, pharmacologic and other organic causes of increased PRL levels, should be followed by detailed diagnosis including MRI. In patients in whom hyperprolactinaemia has been confirmed, the treatment with dopamine agonists (with prevalence of cabergoline, followed by quinagoline) is currently considered first-choice therapy. Surgery should be performed only in those patients resistant or intolerant to these agents, or in patients who refuse long-term therapy. Radiotherapy should be offered only to patients for both pharmacotherapy and surgery have failed, and a role for more modern Gamma Knife radiosurgery should be evaluated.6,7,13,14,27
The future perspectives concern the progress in the medical treatment of prolactinomas resistant to dopamine agonist therapy. There are several potential paths to explore. First, prolactinomas are known to express the somatostatin receptors and are candidates to the treatment with somatostatin analogs. The analogs used nowadays in therapy, octreotide and lanreotide, interact mainly with somatostatin receptors subtype 2 (sst2) whereas PRL inhibition by somatostatin is mediated mostly by subtype sst5.28 Because of that, the attempts of prolactinoma treatment with octreotide or lanreotide were unsuccessful. However, the new analogs, interacting with other receptor subtypes, are under investigation. The in vitro effects of a ‘universal’ somatostatin analog SOM230 on PRL secretion from human prolactinomas are encouraging.29 Another new molecule under consideration is a somatostatin/dopamine chimera acting simultaneously on somatostatin receptors sst2 and dopamine receptors D2. The inhibitory effect of this molecule on PRL secretion from mixed GH/PRL secreting adenomas was recently found.30 The high expression of the nuclear peroxisome proliferator – activated receptors gamma (PPARgamma) in human prolactinomas31 induced us to investigate the effects of PPARgamma agonist, rosiglitazone on estrogen-induced rat prolactinoma cells in vitro.32 The observed inhibitory effect is encouraging, especially because rosiglitazone is a drug vastly used in the treatment of diabetes. However, further studies are still needed. ■