The Management Guidelines for Childhood Differentiated Thyroid Cancer by the American Thyroid Association (ATA) Pediatric Thyroid Cancer Task Force1 built up a system for evaluation, treatment, and follow-up of children with papillary carcinoma. For this approach, recommendations based on scientific evidence and expert opinion play a crucial role in identifying patients at risk of persistent cervical disease and/or distant metastases after initial total thyroidectomy with or without lymph node dissection. In our opinion, this issue needs further consideration because of several uncertainties that have to be addressed.
In fact, children from Belarus, Ukraine, and Russia—an overwhelming majority of whom were exposed to radionuclides at the time of the Chernobyl disaster—are different from their counterparts from other countries.2,3 Our recently published clinically relevant studies support and add important information to the previous experiences:4 children and adolescents with papillary thyroid carcinoma in the ‘post-Chernobyl’ group differed in many clinical and pathologic parameters from those in the ‘sporadic’ group, e.g. lateral nodal disease and distant metastases were significantly more often noted only in post-Chernobyl patients operated on during the early (4-9) and intermediate (10–12) years latency periods.5 However, we argue with the task force’s opinion that important dissimilarities preclude generalization of the clinical and pathomorphologic presentation of post-Chernobyl pediatric papillary thyroid carcinomas to their sporadic counterparts.
Nevertheless, the results of our investigations on internally irradiated patients still have strong points that are relevant to the issue of treatment of childhood thyroid cancer in general, irrespective of radiation exposure.
First, our cohorts6 encompass more than 1000 cases of papillary thyroid carcinoma in patients who were ≤18 years of age at presentation (thus the 20-year treatment results were evaluated in 1078 post-Chernobyl Belarus patients). A comparative analysis of overall, event-free and relapse-free survival did not reveal any significant differences between sporadic and post-Chernobyl cohorts of Belarus patients.6,7 Our results support previous published data from Russia that papillary thyroid carcinomas developed after internal exposure to radioiodine does not display specific risk factors for recurrence that are different from those in sporadic papillary thyroid carcinoma.8 Therefore, common treatment approaches for patients with papillary thyroid carcinoma should be recommended, regardless of history of radiation exposure. For that reason, in our opinion, to disregard clinically relevant conclusions on post-Chernobyl papillary thyroid carcinoma is not appropriate.
The American Thyroid Association Pediatric Thyroid Cancer Treatment Guidelines risk-level groups were defined according to the tumor stage at diagnosis. Unfortunately, references are missing addressing the definitions of ‘microscopic metastasis,’ ‘a small number of neck lymph nodes,’ and ‘regionally extensive disease’; besides, no information how to apply this three-step system to the data of other researchers (there is no formula or algorithm, for example). Of interest, tumor size or minimal extra-thyroid extension, lymphovascular or blood vessel invasion or any other wellknown histologic adverse factors are not mentioned in this scheme too.
Our approach, which proposes evaluation of patients with post-Chernobyl papillary thyroid carcinoma,5,6 is based on demographic, morphologic, and clinical risk factors for extra-thyroid tumor extension, nodal disease, and distant metastasis. It can easily be adapted to any etiologically different group of children and adolescents for planning of initial treatment and post-operative surveillance. In addition, we proved that the risk of recurrence largely depended on the type of surgery (total thyroidectomy versus any other surgical intervention) that influenced the cumulative incidence of both loco-regional and distant relapses of papillary thyroid carcinoma in exposed children.
The proponents for total thyroidectomy usually argue that this intervention helps to stage papillary thyroid carcinoma, as well to prepare patient for radioiodine treatment. The clinical situation in children is more complicated: we should consider that children and adolescents with papillary thyroid carcinoma have a substantial risk for extra-thyroidal extension. For example, in a cohort of sporadic papillary thyroid carcinoma,9 45.5% of patients had extra-thyroidal extension (and 27.3% of a subgroup of patients with tumors sized ≤10 mm) and/or lymph node metastasis.5 In our study5 nodal disease was revealed in 71.6% of patients with sporadic papillary thyroid carcinoma (and 62.5% of a subgroup of patients with tumors sized ≤10 mm. Currently, there is no technique to identify extra-thyroidal extension and/or lymph node metastasis unambiguously; therefore, these risk factors for recurrence cannot be detected/excluded prior to surgery. As a result, we propose to definitely place all patients aged ≤18 years in the moderate-risk group and those who were diagnosed with lateral nodal disease in the high-risk group.
Finally, we want to add different perspectives with respect to risk levels in children with papillary thyroid carcinoma.
• Total thyroidectomy is the only initial surgical approach. A small unilateral tumor in the thyroid should not be treated alternatively because the pre-operative evaluation cannot discriminate between papillary thyroid carcinoma confined to the gland and a neoplasm with minimal extra-thyroid extension.
• We agree that pediatric-specific protocols should be used to minimize ionizing radiation exposure. Therefore, if compartmentoriented central and ipsilateral lymph node dissection was not performed during initial surgery, risk of nodal disease based on age and morphological specifications should be evaluated to decide on the next step of surgery.6 For example, in our experience in many cases of diffuse sclerosing variant of papillary thyroid carcinoma or in patients with a tumor located in close proximity to the isthmus and accompanied by intra-thyroid lymphogenic psammoma bodies dissemination, central and bilateral cervical lymph node metastases occurred.
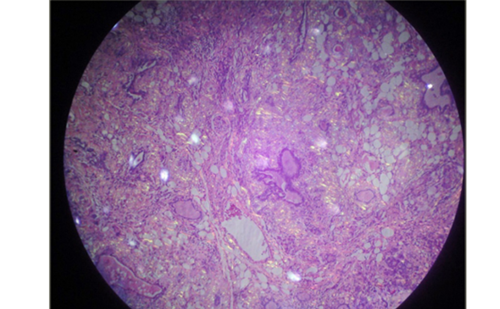
• Treatment of childhood carcinoma needs special expertise not only by a high-volume thyroid surgeon as recommended by the ATA Task Force but morphologic evaluation of tumor tissue by an experienced thyroid pathologist too specialized in childhood thyroid carcinomas. Thus, the ATA Task Force stated that subtypes of papillary thyroid carcinoma in pediatrics include four variants. This classification needs to be amended: for example, in our cohort of patients we distinguished mixed or conventional patterns, that is, admixtures of the solid and follicular variants, although solid, follicular, and papillary patterns could also coexist; in addition, papillary and solid or papillary and follicular patterns could occur.4–6 Warthin-like, tall cell and cribriform variants are not exceptional either.5,6
• Vascular invasion, age at presentation, and exclusion of radioactive iodine therapy from the management increased the risk of distant relapses in children after total thyroidectomy. Therefore, children and adolescents with papillary thyroid carcinoma could be separated into two additional risk groups: those who have the aforementioned characteristics (high risk) and those who are not (low risk).
In conclusion, we call for a reconsideration of the risk levels published by the ATA Pediatric Thyroid Cancer Task Force and propose to integrate data on post-Chernobyl papillary thyroid carcinomas in future management guidelines for children with this type of tumor.