Thyroid nodules are a common clinical problem and with the growing use of diagnostic imaging, the number of thyroid nodules identified and undergoing further diagnostic evaluation by fine-needle aspiration biopsy (FNA) is steadily growing. Only 5 % of all thyroid nodules harbour malignancy and thyroid cancer constitutes only 1 % of all epithelial malignancies worldwide and represents 95 % of all endocrine malignancies.
Thyroid nodules are a common clinical problem and with the growing use of diagnostic imaging, the number of thyroid nodules identified and undergoing further diagnostic evaluation by fine-needle aspiration biopsy (FNA) is steadily growing. Only 5 % of all thyroid nodules harbour malignancy and thyroid cancer constitutes only 1 % of all epithelial malignancies worldwide and represents 95 % of all endocrine malignancies. Thyroid cancer incidence has more than doubled in the past decade, with an associated rise in mortality.1,2 It is currently unknown whether the increase in papillary thyroid cancer (PTC) is real or is an artefact of improved diagnostic techniques and other procedures, or of increased screening for small nodules. Differentiated thyroid carcinoma (DTC), which includes PTC, follicular and poorly differentiated carcinomas, accounts for approximately 95 % of all thyroid cancer cases1 and most patients with DTC have an excellent prognosis;3,4 however, recurrence is observed in 10–15 % of patients following surgery.1
Following the spirit of concrete cultural and scientific integration among the countries participating in the new reality of the EU, the European Thyroid Association and also the American Thyroid Association have endorsed the implementation of a consensus and guidelines for the management of thyroid nodules and thyroid cancer.5,6
Medullary thyroid cancer (MTC) is a malignancy of the parafollicular C cells of the thyroid and accounts for up to 5 % of all thyroid cancer cases, but causes a disproportionate number of thyroid cancer-related deaths. MTC occurs in both sporadic and hereditary settings, the latter accounting for approximately 25 % of MTC cases. The hereditary form of MTC occurs as a component of the autosomal, dominantly inherited cancer syndromes, multiple endocrine neoplasia type 2A, multiple endocrine neoplasia type 2B and familial MTC and is the most common cause of death in patients with these syndromes.7
Anaplastic thyroid carcinoma (ATC) is by far the most deadly of thyroidderived tumours, but fortunately accounts for but a small percentage. In the US, ATC is responsible for 1.7 % of all thyroid cancers, while geographically the prevalence ranges from 1.3 to 9.8 %. In several countries, the prevalence of ATC has decreased dramatically, due in part to increased dietary iodine and better management of DTC.8
Recently, the American Thyroid Association endorsed a guideline for management of patients with recommendations for patients with ATC.8 While all thyroid cancer patients require a multi-disciplinary team of specialists for optimal care, the coordinating physician is frequently an endocrinologist who has established a long-standing relationship with the patient who has DTC or MTC. By contrast, the sudden onset and explosive course of ATC necessitates immediate involvement by surgeons, radiation and medical oncologists, and palliative care teams.
Diagnostic Approach to and Treatment of Thyroid Nodules
Thyroid nodules are the clinical manifestation of a wide spectrum of thyroid diseases. In a normal gland or a diffuse goiter, thyroid nodules may be solitary or multiple. Among multi-nodular goiters, one nodule may become clinically dominant in terms of growth, dimension and functional characteristic. The aim of the diagnostic approach to thyroid nodules is a differential diagnosis between benign and malignant nodules and, in the event of malignancy, the selection of an appropriate surgical procedure.5–7
When a thyroid nodule is detected in a patient by physical examination or incidentally during some other test, the diagnostic steps to follow are: 1. A complete history and physical examination focusing on the thyroid gland and adjacent cervical lymph nodes should be performed. It is important to consider history of familial thyroid cancer, of exposure to radiation during childhood, of rapid growth, hoarseness, hard and irregular consistency, ipsilateral cervical lymphadenopathy and fixation of the nodule to extrathyroidal tissues in a physical exam of the thyroid and neck. 2. Neck and thyroid ultrasound. 3. Thyroid function analysis: thyroid stimulating hormone (TSH), T4 and anti-thyroid antibodies. 4. FNA cytology: when nodule is bigger than 1 cm and/or echographic signs of suspect are present. FNA is the procedure of choice in the evaluation of thyroid nodules. Echographic guidance for FNA is recommended for those nodules that are non-palpable, predominantly cystic or located posteriorly in the thyroid lobe. If FNA or biopsy of a thyroid mass is positive to malignancy and no distance extension is documented, surgical treatment is the first option. If the serum TSH is subnormal, a radionuclide thyroid scan should be performed using either technetium 99 mTc pertechnetate or 123I.5,6
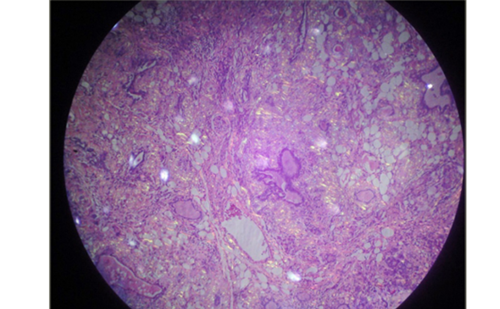
Approximately 15 to 30 % of thyroid nodules evaluated by means of FNA are not clearly benign or malignant. In a recent study, a novel diagnostic test that measures the expression of 167 genes in the cytological sample has shown promise in improving pre-operative risk assessment; of the 265 indeterminate nodules, 85 of those were malignant. The gene-expression classifier correctly identified 78 of the 85 nodules as suspicious, with a sensitivity of 92 % and with a specificity of 52 %. The negative predictive values for atypia (or follicular lesion) of undetermined clinical significance, follicular neoplasm or lesion suspicious for follicular neoplasm or suspicious cytologic findings were 95 %, 94 % and 85 %, respectively. The data of the study suggest consideration of a more conservative approach for most patients with thyroid nodules that are cytologically indeterminate on FNA and benign according to gene-expression classifier results.9
Surgical Treatment
The surgical treatment of DTC approach can be as follows: 1. Total or subtotal thyroidectomy. The most common and recommended approach, especially in the presence of poor prognostic factors (size larger than 4 cm, extrathyroidal extension, bilaterality, age older than 45 years, presence of lymph node metastases). 2. Lobectomy or isthmusectomy. This can be considered in unilateral lesions in the absence of adverse prognostic factors. In case of margin involvement, thyroidectomy should be completed later. Lobectomy may be associated with a higher rate of local recurrence.
Indication of lymph node dissections can be considered in case of palpable cervical nodes or positive biopsy. It will be radical or functional according to tumour extension. In cases of non-palpable lymph nodes, the usefulness of prophylactic lymphadenectomy is unclear, as its value has not been proven. Therapeutic central-compartment (level VI) neck dissection for patients with clinically involved central or lateral neck lymph nodes should be included to provide clearance of disease from the central neck. Prophylactic central-compartment neck dissection (ipsilateral or bilateral) may be performed in patients with papillary thyroid carcinoma with clinically involved central neck lymph nodes or in advanced primary tumours (T3 or T4 stages). Near-total or total thyroidectomy without prophylactic central neck dissection may be appropriate for small (T1 or T2), non-invasive, clinically node-negative papillary thyroid carcinoma and most follicular cancer. 5–7,10
There are several widely used thyroid cancer stages. Application of the American Joint Committee on Cancer/International Union Against Cancer (AJCC/UICC) classification system based on pathological tumour–node–metastasis (pTNM) parameters and age is recommended for tumours of all types. This classification is currently used and is based on the TNM system, taking into account the variables primary tumour size (T), presence of node metastasis (N) and distance metastases (M).
Tumour – Node – Metastasis (PTNM)
Tumour
T0 – no evidence of primary tumour; T1a – tumour 1 cm or less, T1b – tumour more than 1 cm, but not more than 2 cm; T2 – tumour more than 2 cm, but not more than 4 cm, in greatest dimension limited to the thyroid; T3 – tumour more than 4 cm in greatest dimension limited to the thyroid or any tumour with minimal extrathyroid extension; T4a – tumour of any size extending beyond the thyroid capsule to invade subcutaneous soft tissues, larynx, trachea, oesophagus or recurrent laryngeal nerve; T4b – tumour invades prevertebral fascia or encases carotid artery or mediastinal vessels. All ATC are considered T4 tumours. T4a – intrathyroidal ATC – surgically resectable. T4b – extrathyroidal ATC – surgically unresectable.
Node metastasis
NX – regional lymph nodes cannot be assessed; N0 – no regional lymph node metastasis; N1 – regional lymph node metastasis; N1a – metastasis in ipsilateral cervical lymph node(s) – metastasis to level VI (pre-tracheal, paratracheal and pre-laryngeal/Delphian lymph nodes); N1b – metastasis to unilateral, bilateral or contralateral cervical or superior mediastinal lymph nodes.
Distant metastasis
MX – distant metastasis cannot be assessed; M0 – no distant metastasis; M1 – distant metastasis.11,12
Post-operative Treatment
Post-operative 131I remnant ablation is used to eliminate the post-surgical remnant/post-operative residual thyroid tissue. It may facilitate the early detection of recurrence based on serum thyroglobulin measurement and/or 131I whole body scan uptake. Additionally, the post-therapy scan obtained at the time of remnant ablation may facilitate initial staging by identifying previously undiagnosed disease, especially in the lateral neck. The primary goals of the first dose of 131I after total thyroidectomy are: to destroy the residual thyroid tissue and/or any remaining residual tumour; to discover occult disease and be able to establish initial stage; to decrease the risk of recurrence and disease-specific mortality by destroying suspected, but unproven metastatic disease (as an adjuvant therapy); and to treat known persistent disease.13,14
In low-risk patients, some questions remain unresolved: What is the optimal protocol for post-operative 131I administration? In which lowrisk patients should 131I be administered? To answer these questions, two prospective randomised trials (ESTIMAL and HILO) on large series of patients who have been treated with total thyroidectomy have been performed.
In the first (ESTIMAL), a randomised, phase III trial, two thyrotropinstimulation methods (thyroid-hormone withdrawal and use of recombinant human thyrotropin) were compared and two 131 I doses (1.1 GBq and 3.7 GBq) in a two-by-two design. Inclusion criteria were an age of 18 years or older; total thyroidectomy for DTC; PTNM stage, ascertained on pathological examination of a surgical specimen, of pT1 (with tumour diameter ≤1 cm) and N1 or Nx, pT1 (with tumour diameter >1 to 2 cm) and any N stage or pT2N0 and absence of distant metastasis. Thyroid ablation was assessed eight months after 131I administration by neck ultrasonography and measurement of recombinant human thyrotropin-stimulated thyroglobulin. There were 752 patients enrolled between 2007 and 2010 – 92 % had PTC. In the 684 patients with data that could be evaluated, ultrasonography of the neck was normal in 652 (95 %) after 131 I treatment – the stimulated thyroglobulin level was 1 ng/ml or less in 621 of the 652 patients (95 %) without detectable thyroglobulin antibodies. Thus, thyroid ablation was complete in the 92 % of patients and the ablation rate was equivalent between following either 30 mCi (1.1 GBq) or 100 mCi (3.7 GBq) of 131I and similar in the patients treated with recombinant human thyrotropin alpha group versus in the group undergoing thyroid-hormone withdrawal.15
In the second study (HILO), at 29 centres in the UK, a randomised trial comparing low-and high-dose 131I also was conducted, each in combination with either thyrotropin alpha or thyroid-hormone withdrawal before ablation. Patients (age range 16–80 years) had tumour stage T1 to T3, with possible spread to nearby lymph nodes but without metastasis. Endpoints were the rate of success of ablation at 6–9 months, adverse events, quality of life and length of hospital stay. A total of 438 patients underwent randomisation; success rates were 85 % in the group receiving low-dose 131I versus 88.9 % in the group receiving the high dose and 87.1 % in the patients treated with TSH alpha group versus 86.7 % in the group undergoing thyroid-hormone withdrawal. The conclusion of both studies is that the use of recombinant human TSH and low 131 I dose (1.1 GBq) for post-operative ablation may be sufficient for the management of low-risk thyroid cancer.15,16
131I use is increasing in the US, with concern over who should receive it, particularly among patients with low-risk tumours. Therefore, reducing the radiation exposure is a major step forwards. The use of recombinant human thyrotropin and low-dose (1.1 GBq) post-operative 131I ablation instead of thyroid-hormone withdrawal will decrease the retention time of 131I and thus the body radiation dose by 60 % for any administered dose and maintains the quality of life of these patients. It will also reduce the length of the stay in a radioprotection ward and sick leave and this will in turn reduce the global cost of treatment.15,16 The question about whether 131I ablation can be safely avoided in low-risk patients is currently being addressed in a randomised trial in the UK.16
Distant metastasis are detected in 10 % of patients at diagnosis and are the major cause of mortality. They are located in the lungs (50 %), bones (25 %), lungs and bones (20 %) or at other sites (5 %). The treatment of persistent, recurrent and metastatic disease, for which surgery is not an option, consists of 131I therapy and levothyroxine therapy to suppress thyroid-stimulating hormone secretion. These treatments provide complete remission in a third of all metastatic patients. Poorly differentiated carcinoma is associated with a higher risk of recurrence and distant metastasis. Furthermore, it has have a low response rate to 131I and, frequently, a rapid rate of progression.
There are currently no effective therapies for DTC patients who fail to respond to 131I treatment, with conventional chemotherapy so far proving relatively ineffective.17–19 These findings led to the definition of refractory thyroid carcinoma that is observed in patients with: 1. At least one target lesion with no detectable 131I intake. 2. Progression during the 12 months following a 131I treatment. 3. Persistent disease after the administration of 600 mCi (22 GBq) of 131I.20
In the case of advanced tumours refractory to 131I therapy, there are four treatment options: 1. Radiotherapy can be used with radical or palliative aims in both primary tumour or metastatic sites. 2. Treatment with chemotherapy. The only approved cytotoxic drug for use in thyroid cancer is doxorubicin, which results in response rates between 17 and 25 % in uncontrolled studies with few patients and unreliable data. In one of them, in combination with cisplatin, an increase in response rate was obtained without impacting survival. 3. Surgery of metastasis may also be useful in exceptional cases such as single brain metastasis or acute complications such as spinal cord compression. 4. TSH suppression can be useful in keeping serum TSH levels below 0.1 U/ml. In any case, responses to these four approaches are partial and transient with no prolongation of survival. So, molecular-targeted therapies, anti-angiogenic agents and other treatments are being studied.20,22 In a recent study pretreatment with selumetinib increases 131I uptake and retention in patients with thyroid cancer that are refractory to 131I; consequently the effect may be greater in patients with RAS mutant cancer.21
Thyroid-stimulating Hormone Suppression
The use of thyroxine following surgery is performed for two purposes: 1. Replacement purposes of thyroxine in order to preserve thyroid function. 2. Reducing TSH secretion, to avoid its effect as a growth- and proliferation-stimulating factor of tumour cells. The effectiveness of this treatment in preventing recurrence after surgery has been controversial; however, a recent meta-analysis showed a preventive effect on avoiding clinical adverse effects. The purpose of TSH suppression is to obtain serum TSH levels between 0.1 and 0.5 μU/ml in tumour stages II and III, and less than 0.1 U/ml in high-risk tumours for at least five years.23
Treatment of Medullary Thyroid Carcinoma
When a FNA or biopsy of a thyroid mass is positive to MTC and no distance extension is documented, surgical treatment is the first option. It is important to determine the rearranged during transection (RET) proto-oncogene mutation in order to distinguish whether it is a sporadic case or a family syndrome. In the presence of a genetic mutation it is necessary to exclude the presence of pheochromocytoma or parathyroid hyperplasia, in order to treat them appropriately also. In cases of known mutations in RET in early childhood, prophylactic thyroidectomy can be recommended.7 The initial surgery is mainly total thyroidectomy. Level VI and ipsilateral levels II–V lymphadenectomy are also indicated. If any of these nodes are involved or the basal levels of calcitonin are greater than 400 pg/ml, contralateral dissection should be considered. Post-operative radiotherapy may be considered in T4 tumours or those with positive margins. In case of relapse after initial treatment, if disease is localised or it is a solitary metastasis, the treatment of choice is surgery followed or not by radiotherapy. In case of relapse with unresectable localised disease, two options can be addressed: 1. Palliative radiotherapy. 2. Radiofrequency ablation or embolisation. When the disease is no longer a candidate for local treatment, or in case of distant metastases, two treatment options can be considered: 1. Chemotherapy: The approved cytotoxic drug for its use is doxorubicin, which gives response rates between 15 and 25 % in uncontrolled studies with few patients and unreliable data. In this tumour type, responses to treatment with dacarbazine and 5-fluouracil, doxorubicin-streptozocin and dacarbazinedoxorubicin-cyclophosphamide have also been described.24–27
Treatment of Unresectable or Distant Metastatic Relapse
Recently, multi-targeted kinase inhibitors have emerged as promising treatments for differentiated thyroid cancers. Striking and durable disease regression has been induced in many patients treated with these drugs based on mutation detection in samples from thyroid cancer with the addition of BRAF mutation, and also the detection of RAS, RET/PTC and PAX8/PPARγmutations, which may also contribute to cancer diagnosis. On the other hand, the mitogen-activated protein kinase/extracellular signal-regulated kinase signalling pathway (MAPK/ ERK) and lipid kinase phosphoinositide-3-kinase signalling pathway (PI3K/Akt) play an important role in the transmission of cell signals. The genes, coding the signalling cascade proteins (RET, RAS, BRAF, PI3K, PTEN, AKT), are mutated or aberrantly expressed in thyroid cancer derived from follicular thyroid cells. Genetic and epigenetic alternations, concerning MAPK/ERK and PI3K/Akt signalling pathways, contribute to their activation and interaction as a consequence of malignant follicular cell transformation. The understanding of this molecular mechanism provides access to novel molecular prognostic and therapeutic strategies for inhibiting the oncogenic activity of the signalling pathways.22,28 This ability to investigate tumour biology would allow for the selection of different drugs. Several potential targets for therapy have been defined in DTC and MTC and represent new therapies for advanced thyroid carcinoma; on the other hand, experimental cell lines are a novel and invaluable tool that can be used to develop innovative therapeutic approaches to poorly differentiated carcinomas in a pathophysiological context.28–30 After little progress in this field, clinical trials are now studying molecular targeting treatment options for patients who have thyroid cancer metastases that progress despite 131I therapy. There are several aspects or reasons for including patients in these trials: to better define the correct patient population for enrolment in clinical trials; to determine the best therapeutic targets for progressive metastatic thyroid cancer; and to optimise the design so that the appropriate endpoints are measured to best identify the activity that results in the greatest clinical benefit.31
Motesanib,32,33 sorafenib,34 vandetanib,35,36 sunitinib,37 lenvatinib, imatinib and cabozantinib (XL-184)38 are multi-kinase inhibitors that have the ability of inhibiting RET and vascular endothelial growth factor receptor (VEGFR), and other kinases, and have been used in DTC. By contrast, axitinib39 and pazopanib40 seem to act only as anti-angiogenic agents. Nowadays, the most relevant are treatments directed to tyrosine kinase receptors that bind for a wide variety of ligands. Several specific targeted molecules on DTC and MTC are in development, with demonstrated activity in phase II trials.
The proportion of patients achieving partial responses approaches 50 %. However, toxicities from these targeted drugs are substantial, and outcome data available up to this point have all come from singlearm studies. Consequently, important questions about the effects of these treatments on overall disease trajectory and mortality remain unknown. Among these, the only one that has been evaluated in a phase II (DTC) and III (MTC) randomised, placebo trial with demonstrated utility is vandetanib, so this will be the drug of choice when it becomes available.35,36 A phase III trial of cabozantinib (XL184) versus placebo is also finished in MTC and is also available in the US. However, in the absence of approved drugs, off-label use of commercially available drugs, such as sorafenib or sunitinib, is fully justified.41
The results bolster the already substantial body of clinical-response data attained from single-arm trials of kinase inhibitors that suggests progress is being made towards improving outcomes in 131I resistant DTC. Treatment with kinase inhibitors confers risks and potential benefits that, at a minimum, require careful selection of patients. Nevertheless, evidence continues to accumulate to suggest an apparent beneficial role for the use of kinase inhibitors in selected patients who have progressive 131I resistant DTC or in MTC. Although more work is needed to better clarify which patients with differentiated thyroid cancer might have the greatest net benefits from kinase inhibitors.42
Treatment of Anaplastic Thyroid Carcinoma
Patients with ATC who present with a rapidly expanding neck mass require rapid histopathologic confirmation of the diagnosis. There are numerous genetic and epigenetic abnormalities detected by mutations and methylation analyses, array comparative genomic hybridisation (array CGH), microarray, microRNA and protein expression, providing ample opportunities for drug discoveries. If ATC is diagnosed, the patient’s overall clinical status and TNM stage of the tumour should be determined. Treatment goals (aggressive versus supportive care), should be established by disclosing the status and risks/benefits, discussing the patient’s values and preferences, and then having the patient make an informed decision. Patients with stage T4a resectable disease have the best long-term survival, particularly if a multi-modal approach (surgery, intensity-modulated radiotherapy for locoregional control and systemic therapy) is used.43,44 Patients with unresectable stage T4b disease may also respond to aggressive multi-modal therapy. Patients with distant metastases only rarely have responded to traditional therapies, and if an aggressive approach is desired by the patient, a clinical trial should be considered. Hospice or palliative care is also an important component of managing patients with distant metastasis. Healthy patients with localised disease who tolerate full- dose irradiation can potentially benefit from prolonged survival. Current therapeutic options for ATC are unsatisfactory. Surgery followed by chemoradiotherapy can significantly prolong the survival of patients carrying small, intra-thyroidal tumours, but this kind of presentation is very unusual for this cancer. For patients with ATC, the prognosis is very poor, with an overall survival of about 3–6 months. Patients with localised disease not amenable to surgical resection can be treated with neoadjuvant chemoradiotherapy, but the role of this treatment modality is still debated.
There are few active compounds against ATC; the combination of doxorubicin and cisplatin has been the standard for many years. At the present time, paclitaxel plus a platinum compound (often carboplatin) also appears to have efficacy. With regard to biological drugs, axitinib, combretastatin A4, sorafenib and imatinib have been tested in clinical trials, with encouraging activity. The results from several ongoing clinical trials on ATC will hopefully expand the limited therapeutic armamentarium for this deadly disease. A number of thyroid trials have been conducted: combretastatin, sorafenib, pazopanib and AG-013736 (phase II), and PPAR-γ agonist (CS-7017) þpaclitaxel (phase I/II). Four clinical trials were open in Europe (sunitinib, pemetrexed, þpaclitaxel and bevacizumab þdoxorubicin), without preliminary data. The tyrosine kinase inhibitor axitinib also yielded no responses in two treated ATC patients. Gefitinib, an epidermal growth factor receptor–targeted kinase inhibitor similarly produced no responses in five treated ATC patients although one had stable disease for 12 months. However, in a trial of the kinase inhibitor imatinib, two of eight evaluable patients attained a partial response.8
The success of treating ATC will probably require approaches that may involve a comprehensive molecular analysis combining genomewide screening with high throughput screens for druggable targets. Individualised combination therapies that maximally inhibit major pathways and signalling nodes at multiple genetic and epigenetic levels, possibly incorporating developing delivery systems such as gene and virus therapies, and nanoparticles, will hopefully improve the outcome for patients with ATC.45–47
Conclusions
In the last few years, the management of thyroid nodules and thyroid cancer has changed with new perspectives for the future. First, with the implementation of a consensus and a guideline for the management of thyroid nodules and thyroid cancer. Second, with the consideration of a more conservative approach for most patients with thyroid nodules that are cytologically indeterminate on FNA and benign according to gene-expression classifier results. Third, with the results of two studies that propose the use of recombinant human TSH and low 131I dose, 30 mCi (1.1 GBq) for post-operative ablation that may be sufficient for the management of low-risk thyroid cancer. Four, with the knowledge of genes, coding the signalling cascade proteins that are mutated or aberrantly expressed in thyroid cancer. This ability to investigate tumour biology would allow for the selection of different drugs. As consequence, several potential targets for therapy have been defined in DTC, MTC and even in ATC, and these drugs represent new therapies for advanced thyroid carcinoma.