The cytological examination of the thyroid gland is based on microscopic assessment of a material obtained by means of fine-needle aspiration biopsy (FNAB). The main goal of FNAB is to classify the examined lesion as malignant, suspicious or benign and, thus, to select the patients who should be treated surgically. Nowadays, FNAB is a central method in diagnosing pathological lesions in the thyroid gland.
The cytological examination of the thyroid gland is based on microscopic assessment of a material obtained by means of fine-needle aspiration biopsy (FNAB). The main goal of FNAB is to classify the examined lesion as malignant, suspicious or benign and, thus, to select the patients who should be treated surgically. Nowadays, FNAB is a central method in diagnosing pathological lesions in the thyroid gland. It is the examination of choice not only for evaluating thyroid nodules, but also for diagnosing focal lesions revealed by ultrasound (U/S) imaging and for monitoring benign, degenerative and inflammatory lesions and recurrent goitres. There are still discrepancies between authors in the indications for FNAB in small lesions (<1 cm in diameter) found accidentally during U/S imaging of the neck (incidentalomas). In some clinics, patients with such lesions are subjected to FNAB only if risk factors of thyroid carcinoma are present.
Methodology of FNAB of the Thyroid
FNAB of the thyroid is preceded by palpation of the gland and U/S examination. Data from clinical and U/S examinations (including changes in lesion size and consistency, mobility, echogenicity and/or vascularisation pattern) allow the selection of lesions to puncture. U/S-guided biopsy is recommended, as it allows observation of the needle direction in the thyroid tissues. In order to obtain a suitable amount of diagnostic material, some punctures are usually performed in different sites of the altered part of the gland. Typically, physicians use 2–10ml syringes, mounted in an aspirating syringe holder, and needles with an external diameter of 0.4–0.5mm.
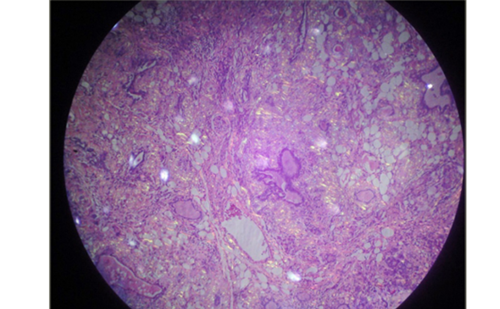
The obtained material is smeared on microscopic slides. When the material is liquid, it is advisable to use the cytocentrifugation technique for aspirate preparation, enabling cell condensation from any residual material left in the syringe. Smears are fixed in 96% ethanol or with fixatives in aerosol and stained with haematoxylin and eosin or by Papanicolaou staining. When May–Grünwald–Giemsa staining is to be applied, the smear should be left to dry.
The methodology of FNAB of the thyroid differs slightly between clinics. In some, no aspiration is performed as the material is obtained without applying any underpressure, with movements of needle – mainly rotations – only. Sometimes, but rarely, needles of a larger diameter are used. It probably allows the physician to obtain more cellular material but, as opponents of such modification indicate, it also increases the number of blood cells in the smears and can result in intrathyroidal haemorrhage. What is more, there are differences in the number of punctures performed. One should remember that the higher the number of punctures, the higher the risk of pathomorphological changes in the thyroid. Such changes make the subsequent cytological or histopathological examinations difficult to interpret (particularly by obscuring the assessment of invasiveness).
Criteria of Diagnostic Smears
During FNAB of the thyroid, non-diagnostic/inadequate aspirates are relatively frequently obtained. The percentage of non-diagnostic specimens has been reported to be between 1.64% and 21%. The differences between the reported rates of inadequate outcomes are mainly a reflection of the non-uniform criteria for the classification of an aspirate as diagnostic. Some authors require five to six groups of well-preserved, well-visualised follicular cells, each group containing 10 or more cells. Others are more rigorous and demand to obtain a minimum of six to eight groups of well-preserved follicular epithelium on each of two slides.
Moreover, the availability of relevant clinical data is an important factor in considering the aspirate as adequate. Even a small number of thyroid follicular cells with typical cytological features of papillary thyroid carcinoma (PTC) could allow the formulation of a strong suspicion of the presence of this carcinoma in a nodule, especially when clinical data are also suggestive. Thus, a strict criterion, based on the number of cells in a smear, is needed to exclude malignancy and not affirm it.
If non-diagnostic material is obtained, the examination should be repeated. However, the data of the Department of Endocrinology and Metabolic Diseases indicate that even non-diagnostic FNAB gives some useful clinical information. The risk of thyroid neoplasm (benign and malignant taken together) is higher when the specimen obtained during aspiration is not diagnostic. If a second biopsy is not performed or is, again, non-diagnostic, the patient should be monitored very carefully and surgical treatment should be considered.
Diagnostic Efficiency of FNAB
The cytological outcome consists of, at least, two parts – the description of material and the diagnostic conclusion. Considering FNAB of the thyroid, the cytological outcome can be classified into several groups, according to the degree of confidence of the diagnostic conclusion:
- Group I – the cytological picture is characteristic enough to make an unequivocal diagnosis of a specific disease entity. This group contains cases of undifferentiated carcinoma, PTC, subacute granulomatous thyroiditis and suppurative acute thyroiditis.
- Group II – a cytological picture with accurate clinical data allows a definite disease entity to be distinguished. This group contains cases of medullary carcinoma, malignant lymphoma, cyst, nodular goitre, metastatic neoplasm and chronic thyroiditis (i.e. Hashimoto’s disease).
- Group III – the cytological picture and clinical data allows the clinician to draw the differential diagnostic circle: follicular neoplasm – follicular tumour; oncocytic tumour; benign tumour – benign lesion; chronic inflammatory reaction. In such cases, formulating the final diagnosis is possible only after post-operative histopathological examination.
- Group IV – the outcome is confined to a description of aspirated material, sometimes with additional remarks on further diagnostic/ therapeutic management.
- Group V – the cytological picture unequivocally indicates that the punctured structure/lesion is not pathologically thyroid but a lymph node, salivary gland, parathyroid, muscular tissue, fat tissue, tracheal element (ciliary (respiratory) epithelium) or teratoma.
It should be stressed that, in relation to FNAB of other organs, biopsy of the thyroid is burdened with a relatively high proportion of equivocal diagnoses, especially with regard to differentiation of follicular lesions, i.e. carcinomas, adenomas and some hyperplastic nodules in nodular goitre. In these cases, microscopic images do not allow the formulation of a definite diagnosis despite there being a suitable amount of aspirated cellular material, and the cytological outcome only specifies the diagnostic circle, e.g. ‘follicular neoplasm/tumour’. In practice, the decision on thyroid surgery is made based on equivocal FNAB outcomes.
For the optimum use of FNAB of the thyroid, this examination should be performed in centres with experience in thyroid cytology. The necessary condition for reliable outcomes is a control system comprising the comparison of cytological outcomes with the results of post-operative examinations. Such a comparison allows assessment of FNAB efficacy. The sensitivity of FNAB of the thyroid with regard to diagnosing malignancy is reported to be between 65% and 99%, and its specificity between 72% and 100%.
However, the statistical approach to the evaluation of FNAB data varies between authors, making reported results very difficult to compare. Some authors evaluate the sensitivity and specificity of FNAB with respect to diagnosing thyroid neoplasms (regardless of whether they are benign or malignant); others take only malignant neoplasms into account. Yet other authors exclude the socalled intermediate results (differently defined) from statistical analysis.
Methods Supporting FNAB of the Thyroid
In order to increase the diagnostic efficacy of the thyroid cytological examination, various methods improving the evaluation of the obtained material have been employed. Some of those methods, including computerised image analysis, add quantitative assessment to routine qualitative evaluation performed by cytopathologists. Other methods employ additional immunocytological or other specific staining. These methods allow the clinician to determine the detailed histogenesis of aspirated cells and, in some cases, to distinguish between malignant and benign lesions. Molecular biology techniques are also used for this purpose.
Computer-aided Analysis of Routine Smears
Computerised karyometric analysis allows quantitative evaluation of the size, shape and, occasionally, some other features of cell nuclei on routinely stained smears. It has been found that the assessment of the mean size of thyrocyte nuclei is of limited value.
However, the assessment of the level of anisokaryosis is useful in diagnosis of follicular lesions. The level of anisokaryosis in benign lesions (apart from recurrent goitre) was significantly lower than in malignant neoplasms. Karyometric analysis also proved the necessity of considering the age and sex as well as the thyrometabolic state of the patient and the history of treatment while evaluating the microscopic image.
The usefulness of joint karyometric and cytophotometric analysis (DNA contents evaluation) has also been assessed. However, the presence of aneuploidy in part of the follicular adenomas and hyperplastic nodules have been shown, which indicates that DNA analysis cannot be used for the differentiation between neoplastic and non-neoplastic lesions. Moreover, the use of DNA histogram analysis, together with karyometric evaluation, does not improve the accuracy of karyometry in diagnosing malignant thyroid neoplasms.
Methods Based on Additional Staining
Various antigens have been tested for immunocytological staining of thyroid smears. None of them allows the main limitation of FNAB of the thyroid gland to be overcome, i.e. to distinguish follicular neoplasms. For example, it has been shown that peroxidase in thyroid carcinoma cells does not contain all epitopes, and it does not bind the murine antibody MoAb47 – contrary to the cells from benign lesions. However, it has been found that false positive staining with that antibody is relatively frequent.
Until recently, there was focus on galectine, but detailed studies have shown that this marker is not effective if features of chronic thyroiditis are present. On the other hand, it has been found that examination of cytokeratin 19 expression may be useful in diagnostically difficult cases of PTC.
The usefulness of the analysis of argyrophilic proteins related to nucleolar organising regions (AgNOR), reflecting the rapidity of cell proliferation, has also been assessed. The NOR silver-staining technique can be performed on de-stained cytological slides (e.g. previously stained with haematoxylin and eosin), which eliminates the need for additional punctures.
The evaluation of variables describing the area of AgNOR dots could be useful in the diagnostics of thyroid lesions. Among the analysed variables, it was the total area of dots in the nucleus that presented with the highest discriminating value in follicular lesions distinctions.
Molecular Markers
Molecular markers used in techniques supporting FNAB of the thyroid can be divided into tissues-pecific, such as sodium/iodide symporter (NIS), thyroperoxidase (TPO) or thyroglobulin (Tg), and cancer-specific, such as re-arranged during transfection proto-oncogene (RET) re-arrangements. Tissue-specific markers allow confirmation of the presence of thyroid follicular cells in a smear and, when a lymph node is punctured, confirmation of metastasis. Cancer-specific markers can be used to diagnose malignancy.
With the reverse transcription polymerase chain reaction (RT-PCR) technique, the specific gene expression can be shown even in very scarce material obtained through washing out of the needle after a routine smear. This is an important advantage, allowing early diagnosis of cancer recurrence in lymph nodes by revealing messenger RNA (mRNA) for thyroglobulin when routine cytological examination does not show the presence of thyroid follicular cells in the nodule; mRNAs for thyroid-stimulating hormone (TSH) receptor, NIS, iodothyronine deiodinases and TPO have also been reported to be evaluated in the material obtained by FNAB.
Cancer-specific markers prove malignancy of examined lesions. In the thyroid, rearrangements of RET/PTC, characteristic of PTC, have most frequently been evaluated. Searching for multiple molecular markers in thyroid aspirates (RET/PTC and activating mutations of the v-raf murine sarcoma viral oncogene homologue B1 (BRAF) gene) may enhance the accuracy of FNAB and refine the preoperative diagnosis of PTC. This method can be useful, particularly in cases in which the obtained material is too scarce for routine cytology.
The expression of telomerase, high-mobility group I protein (HMGI), paired box gene 8 peroxisome proliferator activated receptor (PAX8-PPAR) gamma 1 rearrangements, galectin and CD44 (a polymorphic family of immunologically related integral membrane glycoproteins associated with cell matrix adhesion) were also examined in thyroid aspirates.
Conclusions
FNAB is a reliable method for the evaluation of pathological lesions in the thyroid if its limitations are properly approached. Thus, FNAB of the thyroid should be performed in centres with sufficient experience in this field and in which cytological outcomes are compared with post-operative histopathological results. The possibility of molecular evaluation of aspirated material opens new horizons for FNAB of the thyroid. ■
A version of this article, with references, can be found in the Reference Section on the website supporting this business briefing (www.touchbriefings.com).