Summary
An interesting case of persistent hypercalcaemia of primary hyperparathyroidism (pHPT) resistant to medical management for more than 5 years, who demonstrated a dramatic response to the first dose of denosumab with a significant and persistent drop in her level of calcium, from a baseline of 3 mmol/l to 2.7 mmol/l over a period of 9 months.
Summary
An interesting case of persistent hypercalcaemia of primary hyperparathyroidism (pHPT) resistant to medical management for more than 5 years, who demonstrated a dramatic response to the first dose of denosumab with a significant and persistent drop in her level of calcium, from a baseline of 3 mmol/l to 2.7 mmol/l over a period of 9 months.
Background
A 90-year-old patient who had been followed up in our endocrinology department for 5 years with a diagnosis of pHPT. The medical history included hypertension, congestive cardiac failure secondary to ischaemic heart disease and chronic kidney disease stage III. There was no current or past medical history of renal stones and the patient had never smoked.
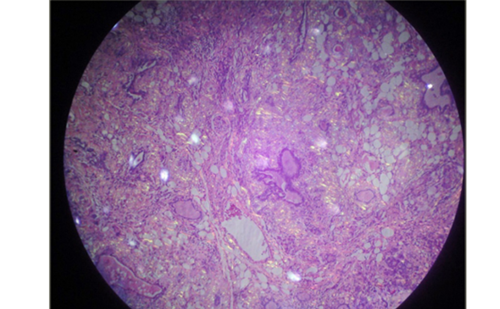
The possibility of familial hypocalciuric hypercalcaemia was ruled out by normal 24-hour urinary calcium excretion levels. No evidence of a parathyroid adenoma on imaging nor any evidence of malignancy or multiple myeloma. Dexa scan not performed.
Renal function was stable with epidermal growth factor receptor (eGFR) between 50 and 60 (stage III) and a normal thyroid function and vitamin D levels.
Case Presentation
The patient had been noted to have persistent elevated serum calcium levels (baseline adjusted calcium 3 mmol/l to 3.1 mmol/l) with a raised parathyroid hormone for the past 5 years, in which time she had remained completely asymptomatic. She had an extensive and thorough work up for hypercalcaemia including a staging computed tomography (CT) scan twice, myeloma screen several times, urinary calcium for familial hypocalciuric hypercalcaemia as well as tests for sarcoidosis that were all reported as normal.
Given this patient’s age and co-morbidities it had been decided that her management for the pHPT should remain non-surgical; however, a myocardial perfusion (MIBI) scan was performed, which had been inconclusive of an adenoma. A trial of cinacalcet was commenced in the past and unfortunately this provoked a type 1 hypersensitivity reaction and therefore had to be discontinued. Subsequently the patient was given a trial of calcitonin nasal spray, which actually successfully reduced the baseline The calcium level of this patient was adjusted to 2.8 mmol/l; however, this was withdrawn from the UK drug market.
The next management step attempted was biphosphonate administration (oral alendronic acid and then zoledronic acid injections), which had no effect in reducing her calcium levels.
With no further treatments available for this patient’s pHPT and persistent hypercalcaemia, we felt it was important to treat while asymptomatic to prevent a medical emergency as her calcium level was persistently above 3 mmol/l and to prevent complications, even though she was although asymptomatic. Her hypercalcaemia proved resistant to oral and intravenous (IV) biphosphonates and it was deemed necessary to trial a UK-licensed medication (denosumab); however, it is unlicensed in this condition. This was discussed with pharmacy and was found to be the preferred method, rather than an unlicensed medication such as calcitonin. This is a medication administered via subcutaneous injection every 6 months and has shown significant reductions in serum calcium levels in patients with hypercalcaemia of malignancy (HCM). In our patient with pHPT her calcium level dropped to 2.6 mmol/l for the first time and persisted at 2.7 mmol/l after 9 months from the initial dose of 60 mg subcutaneously.
Outcome and Follow-up
Follow-up over the 9 months following administration of the initial dose of denosumab – with repeated calcium levels – currently shows a calcium level of 2.7 mmol/l, which is at the higher end of the normal range (with an initial drop to 2.6 mmol/l).
Discussion
Denosumab is a fully human monoclonal antibody that reduces osteoclast-mediated bone destruction by inhibiting the receptor activator of nuclear factor kappa-B ligand (RANKL), a primary mediator of increased osteoclast activity (RANKL levels are elevated in patients with pHPT and correlate positively with rates of bone loss and hypercalcaemia).1
Denosumab is approved for prevention of skeletal-related events in patients with bone metastasis from solid tumour and is recommended as a treatment option for the primary prevention of osteoporotic fragility fractures in postmenopausal women only.2
Medical therapy remains an option for hyperplasia in all glands and for the majority of pHPT patients who are not fit for surgery.2 Cinacalcet has been shown to be a reasonable alternative therapy for non-surgical group of patients; however, it was unfortunately contraindicated in our patient (as she developed angioedema). Limitations in using cinacalcet include an increase in urinary calcium excretion, which is a major risk factor for nephrolithiasis, and it does not demonstrate an increase in bone mineral density,3 unlike denosumab. Furthermore, cinacalcet is administered up to four times a day whereas denosumab is given subcutaneously every 6 months.
Denosumab has proved itself to be superior to biphosphonates in HCM. Hu et al.4 showed that despite IV biphosphonate treatment in patients with HCM, denosumab effectively lowered serum calcium within 10 days in 64 % of patients. Fizazi et al.5 demonstrated, in a study, a reduction in calcium levels in 48 patients receiving denosumab compared with only 13 patients receiving zoledronic acid and there are other studies proving the same advantage of denosumab over biphosphonates (Stopeck et al.6 and Henry et al.7).
Our patient required denosumab as a licensed medication for an unlicensed indication and to our knowledge this is the first case report in the literature to show the possible efficiency and superiority of denosumab over biphosphonates in lowering the calcium level related to pHPT.
Learning Points
- To highlight the potential use of denosumab in patients who are not fit for surgical intervention and who remain resistant to medical management.
- Possible superiority of denosumab over biphosphonates in these cases.
- Denosumab is not licensed yet for this indication; however, more clinical trials are needed to prove the efficiency of denosumab and hence the change in practice.