Thyroid nodules are very common in clinical practice, with an overall prevalence that varies from 4% by palpation to 67% by ultrasonography. The annual incidence by palpation has been estimated at 0.09% by the Framingham study,1 which translates into approximately 300,000 new nodules in the US in 2005. Despite their high frequency, only a small fraction (~5%) of thyroid nodules harbor cancer. Because only malignant or large, symptomatic nodules will require surgical excision, a systematic approach to their evaluation is important to avoid unnecessary surgery.
Thyroid nodules are very common in clinical practice, with an overall prevalence that varies from 4% by palpation to 67% by ultrasonography. The annual incidence by palpation has been estimated at 0.09% by the Framingham study,1 which translates into approximately 300,000 new nodules in the US in 2005. Despite their high frequency, only a small fraction (~5%) of thyroid nodules harbor cancer. Because only malignant or large, symptomatic nodules will require surgical excision, a systematic approach to their evaluation is important to avoid unnecessary surgery. Certain aspects in the evaluation and management of thyroid nodules remain controversial or represent clinical dilemmas.
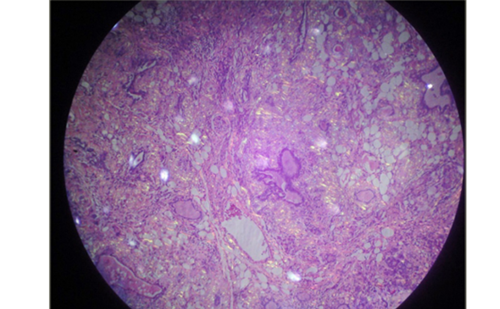
‘ Non – diagnostic ’ Smear
Fine needle aspiration (FNA) biopsy is the most costeffective and accurate method of distinguishing benign from malignant thyroid nodules. This procedure has led to a substantial reduction of unnecessary surgeries, while doubling or tripling the malignancy yield at thyroidectomy. Despite its overall excellent accuracy, approximately 15% of all specimens will be classified as ‘non-diagnostic’ or ‘insufficient’, a diagnosis that poses a management dilemma. Repeat aspiration, preferably under ultrasound guidance, can significantly reduce the rate of non-diagnostic smears. However, when repeat aspiration fails to provide an adequate specimen, the clinician must decide whether to follow the patient clinically or refer for surgical excision. Certain clinical features (history of head or neck irradiation, rapid nodule growth, a hard nodule with fixation to surrounding tissues, compressive symptoms such as dysphagia or persistent hoarseness) increase the likelihood of malignancy in a nodule and may be considered an indication for surgery. However, many patients who lack such clinical features are often found to have thyroid cancer on subsequent evaluation. It is important to recognize that ‘nondiagnostic’ is not synonymous with benign disease, as shown in a study where a 9% incidence of malignancy and a 52% rate of neoplasia was seen after surgical excision of nodules with repeatedly non-diagnostic cytopathology.2 In the presence of ‘high-risk’ clinical features, surgical excision should be considered to definitively exclude malignancy, while observation and re-evaluation in six to 12 months may be appropriate for low-risk patients.
‘ Suspicious ’ or ‘ Indeterminate ’ Cytology
The finding of ‘indeterminate’ or ‘suspicious’ cytologyon FNA biopsy of thyroid nodules is one of the most challenging diagnostic dilemmas for the endocrinologist, and the best management strategy remains controversial. This category includes cytologic findings commonly referred to as ‘follicular neoplasms’ that include hyperplastic nodules, follicular adenomas and carcinomas, and follicular variants of papillary carcinoma.3 The microscopic distinction is difficult, leading most clinicians to recommend surgical excision for a definitive diagnosis. Due to the fact that only 15% to 20% of these lesions will ultimately be found to represent cancer,4,5 up to 85% of patients in this subgroup may undergo unnecessary surgery, with its attendant high cost and potential morbidity. Many studies have attempted to determine factors predictive of malignancy in patients with cytologic findings ‘suspicious for follicular neoplasm’.6,7 Although certain clinical findings (large nodule diameter, fixation to surrounding tissue,male gender, and younger age of the patient) were associated with increased risk of malignancy in some studies,6,7 others found that no cytological,3 clinical, scintigraphic, or ultrasonographic characteristics were predictive of malignancy.8 Other techniques, such as the use of electron microscopy, flow cytometry, and several genetic markers, have been evaluated, but have not improved diagnostic reliability. However, two immunohistochemical markers (HBME- 1 and galectin-3) have shown promise in their ability to predict malignancy and their potential for ease of use in any surgical or cytopathology laboratory, in academic or community settings.9,10 Bartolazzi et al. conducted a retrospective analysis of 618 tissue specimens and 165 cell blocks, as well as a prospective analysis of 226 ultrasound guided (UG)-FNA specimens.9 In the retrospective review of their surgical specimens, 94% of 311 malignant cases stained positive for galectin-3. Less than 3% of papillary carcinomas failed to express this marker.Thirty-seven (93%) minimally invasive follicular thyroid carcinomas were positive for galectin-3, and this marker was not expressed in any case of nodular hyperplasia or thyroiditis. More importantly, the prospective analysis focussed on 90 cases in which conventional cytology was inconclusive. In these cases, the addition of galectin-3 allowed the correct identification of all malignancies, including five minimally invasive follicular carcinomas.
Evaluation of the Patient with Multinodular Goiter
The evaluation of a patient with a palpable solitary nodule is generally straightforward and will usually include FNA biopsy with or without ultrasound guidance. It is important to recognize that in up to 48% of patients with a clinically palpable solitary nodule, ultrasonography will often demonstrate the presence of one or more additional nodules.11 The evaluation and management of patients with multinodular goiters (MNG) represents a much more difficult problem in the clinical setting. It had been suggested that, in the setting of multi-nodularity, a dominant palpable thyroid nodule is most often benign,12 but a study by Belfiore et al.13 found that the frequency of thyroid cancer in patients with a solitary nodule (4.7%) does not differ from that in patients with a non-toxic MNG (4.1%). Because no single clinical or ultrasonographic feature has been found to reliably confirm or exclude the presence of malignancy, selection of the nodule(s) that will require biopsy needs careful consideration. It is generally recommended that in the setting of a multinodular goiter, the dominant nodule should be biopsied. However, certain ultrasonographic features of thyroid nodules, such as hypoechogenicity, the presence of microcalcifications, increased vascular flow, or irregular borders, are associated with increased risk of malignancy14 and, when present, should help the clinical in selecting the target of the FNA biopsy (see Figures 1 and 2). In the absence of these features malignancy cannot definitively be excluded, therefore patients with MNG should be followed with periodic neck
examination and ultrasonography and a repeat biopsy should be considered if significant growth of a nodule is noted or other worrisome clinical (persistent hoarseness, dysphagia, adenopathy, etc.) or sonographic features develop on follow-up.
Therapeutic Considerations in Benign Thyroid Nodules
Thyroid Hormone Suppressive Therapy
For many years, levothyroxine (LT4) has been used by many clinicians at doses sufficient to suppress thyroid stimulating hormone ((TSH) regarded as a growth factor for thyroid epithelial cells), in order to prevent or reduce growth of thyroid nodules. However, this practice is still controversial.
Several randomized studies have concluded that suppressive thyroid hormone therapy results in significant reduction in nodule volume,15–18 but other studies do not support this finding.19,20 Methodological differences in the design of those studies, as well as the heterogeneity of the populations studied, variable treatment doses, duration of therapy, definitions of ‘response’ to treatment, level of TSH suppression, and the methodology used to assess nodule volume (palpation versus ultrasound), are all contributing factors to the discrepant results.
Several meta-analyses, conducted to evaluate the effectiveness of such therapy, have also yielded conflicting results,17,21 although in most at least a trend was seen toward reduction in nodule volume. Because prolonged thyroid hormone suppressive therapy has been associated with adverse effects in the cardiovascular22 and skeletal systems,23 patients must be carefully selected for this therapy and potential risks must be carefully weighed against the expected benefits. If treatment with LT4 is chosen, low level TSH suppression (0.4–0.6mIU/L) should be used.24
Percutaneous Ethanol Ablation
Absolute alcohol has sclerosing properties and causes tissue ablation as a result of a direct coagulative necrosis and local small vessel thrombosis.25 Percutaneous ethanol injection (PEI) has been used over the past two decades as an alternative to surgery in the management of hepatic and renal cysts26,27 and, more recently, in the treatment of primary hyperparathyroidism in patients who are considered poor surgical candidates or who refuse surgical intervention.28 Since the 1990s, several studies evaluated the effectiveness of PEI in the treatment of autonomous29,30 and benign hypofunctioning thyroid nodules and found this treatment to be a suitable alternative to conventional modalities such as surgery or radioiodine ablation.31 However, no controlled randomized studies comparing long-term efficacy of PEI with traditional methods have been conducted. Complete ablation of autonomous nodules is rarely achieved, and in cases of large hyper- or hypofunctioning nodules, multiple injections are frequently required, making this technique time-consuming and less attractive both to physicians and patients. Additionally, side effects and complications, such as pain, laryngeal nerve damage, periglandular fibrosis, or dysphonia, have been reported.32 PEI for treatment of autonomous nodules has been abandoned in most centers given the ready availability and proven efficacy of radioiodine therapy for this indication, with a lower rate of side effects.
Simple thyroid cysts are rare, comprising only about 4% of all thyroid nodules, but up to 32% of surgically excised thyroid nodules have a major cystic component.33 Although cystic thyroid nodules have often been regarded as benign lesions, the cystic nature of a nodule does not necessarily rule out malignancy,33-34 and FNA biopsy, preferably of the solid component or the wall of the lesion, must be performed to exclude a cancerous lesion. Once a cystic nodule has been confirmed as benign, PEI has been proposed as an effective and safe alternative to surgery for these lesions.35–37 A study by Verde et al. demonstrated nodule volume reduction of more than 50% from baseline in 80% of patients treated with PEI, and a significantly lower risk of recurrence at one and 12 months compared with patients treated with simple cyst aspiration.36 Another prospective study in 43 patients who were not eligible or refused surgery for treatment of recurrent thyroid cysts demonstrated that PEI resulted in a greater than 90% nodule volume reduction and alleviation of compressive symptoms in 93% of treated patients.37 Side effects generally included mild local tenderness and transient laryngeal dysfunction. Despite these encouraging results, surgery remains the preferred option in most centers, given the lack of randomized controlled studies in large groups of patients, and the risk of missing cystic papillary carcinomas.38
Ultrasound – guided Laser Thermal Ablation
Although surgical excision remains the standard treatment for benign hypo-functioning thyroid nodules that are associated with compressive symptoms, many patients are poor surgical candidates or refuse such intervention. Alternative treatment modalities, such as suppressive LT4 therapy or PEI are not always effective and may be associated with unacceptable side effects in many patients. Ultrasound-guided laser thermal ablation (LTA) has emerged in recent years as a novel therapeutic option in the management of these patients. LTA has been successfully used in the palliative management of primary and metastatic liver tumors,39–41 renal tumors,42 and, more recently, in the management of benign cold and hyper-functioning thyroid nodules.43–44 The procedure involves the delivery of light directly into the tissues via a laser fiber, resulting in photocoagulation due to the increase in temperature (>100ºC) within the involved lesion. Pacella et al. initially demonstrated the utility of this technique by applying it immediately after excision to 18 thyroid glands, obtained from patients who had undergone thyroidectomy for Graves disease or large goiters, and subsequently in two volunteers about to undergo thyroidectomy for large hyper-functioning thyroid nodules.45 Subsequent studies have demonstrated significant nodule volume reduction with resolution of compressive symptoms and of hyperthyroidism in patients with large benign cold or autonomous thyroid nodules.43,44 The only significant side effect included transient burning cervical pain, occasionally requiring treatment with corticosteroids.46 The procedure requires significant skill on the part of the physician and is currently only available in selected centers in Europe.These reported series are small, and further randomized controlled studies are needed to compare results of this new technique with other conventional treatment modalities before such therapy can be recommended.
Conclusions
Although thyroid nodules are very common in clinical practice, the majority represent benign lesions. To avoid unnecessary surgery with its associated risks, high cost, and potential morbidity, a systematic approach to their evaluation is recommended. Several aspects in the evaluation and management of thyroid nodules remain a challenge and the best approach is not always straightforward. The ‘non-diagnostic’ specimen, particularly after repeat aspiration under ultrasound guidance, and those nodules classified as ‘suspicious for follicular neoplasms’ represent some classical examples.When a benign diagnosis cannot be confirmed with FNA biopsy, surgical excision is usually recommended. However, only a minority of these nodules will ultimately be found to harbor malignancy. Most studies to date have failed to identify reliable predictors of malignancy in this subset of patients, but some immune-histochemical markers have shown initial encouraging results that will need further confirmation before their use in clinical practice can be generally recommended.
The use of suppressive doses of LT4 in patients with benign thyroid nodules with the purpose of inducing reduction in nodule volume remains controversial.The potential adverse effects of prolonged LT4 suppressive therapy in the cardiovascular and skeletal system need to be weighed against their perceived benefit. PEI and LTA have been used successfully in some centers in the treatment of benign cystic and solid thyroid lesions, particularly in patients who have been deemed poor surgical candidates or those who have otherwise refused the more conventional surgical approach. Reported side effects of these treatment modalities have generally been mild and transient. Both of these techniques require significant skill on the part of the operator and are often not readily available. Furthermore, additional large randomized studies comparing the long-term efficacy of these novel approaches with conventional surgical treatment are needed before such therapies can be widely recommended.■