- Varo—a person dealing with things sensibly and realistically in a way that is based on practical rather than theoretical considerations (Urban Dictionary).
- Város—weight, burden, overweight (Greek).
- Vero—merchandise, trade good (Esperanto).
The phrase “patient-centered” defines modern diabetes care, and rightfully so.1 In patient-centered diabetology, the patient’s specific needs and requirements are taken into consideration while planning therapy. This helps achieve glycemic targets in a safe and well-tolerated manner. Current guidelines try to match the framework set by accepted definitions of patient centered care, as well as the bio-psychosocial model of health.2,3
The American Diabetes Association/European Association for Study of Diabetes (ADA/EASD) provide a horizontal choice of second-line drugs, and third-line combinations, to be prescribed in case of metformin inadequacy.1 It is clear that pleiotropic benefits, rather than efficacy per se, inform the choice of treatment. This style leaves the selection of a particular drug class (or classes) to the treating physician. For the student, or inexperienced caregiver, such a guideline does not assist in deciding techniques, tactics, and troubleshooting while treating diabetes.
The American Association of Clinical Endocrinology/American College of Endocrinologists (AACE/ACE) try to simplify matters by proposing a vertical hierarchy of drug classes.4 Here, glucose-lowering drugs are listed in descending order of appropriateness, based upon safety and tolerability. The main criterion for ranking seems to be the effect on weight, as weight loss is clearly mentioned, along with achievement of euglycemia, as a targeted outcome in type 2 diabetes care. Such a rubric, however, ignores the needs of underweight, lean, and normal-weight persons with diabetes.
To assist in clinical decision-making, we have proposed the concept of metabolic triage,5 based upon the metabolic fulcrum. In this model, persons with type 2 diabetes are triaged into three categories: eubolic, extremely catabolic, and maladaptive anabolic. This classification is based upon phenotype, and is backed by insights from pathophysiology, biochemistry and endocrinology.6,7 A type 2 diabetes person in catabolism will have predominant insulin deficiency, with a low insulin/glucagon ratio, and AMP-activated protein kinase (AMPK) hyperactivity. A maladaptive anabolic individual, on the other hand, will be predominantly insulin resistant, have a high insulin/glucagon ratio, and require AMPK activation. These factors help in choosing appropriate glucose-lowering treatment,5 including injectable therapy.8
The metabolic fulcrum is a simple, yet effective, clinical aid, as well as a pedagogic tool. We strengthen this further by proposing a váro-centric model of diabetes care. In Greek, “város” means weight or heaviness.9 As per the Urban Dictionary, varo is “a person dealing with things sensibly and realistically in a way that is based on practical rather than theoretical considerations”.10 In Esperanto, “varo” implies ware, trade goods, or merchandise.11
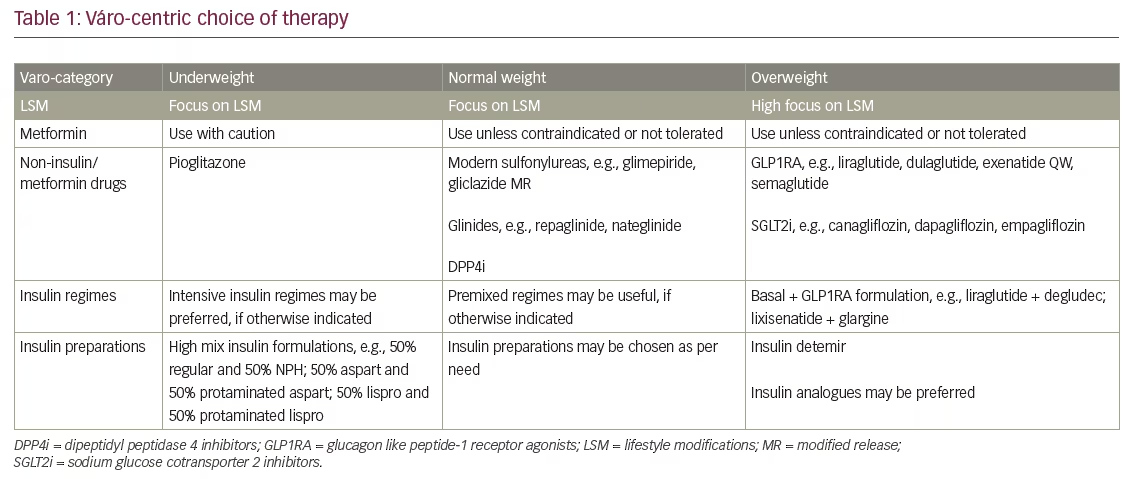
The váro-centric model of diabetes care suggests practical usage of available therapeutic options, based upon the weight (or body mass index) of the person with type 2 diabetes (Table 1). Such a model takes the needs of the individual person with diabetes into consideration, while promoting use of “good clinical sense”,12 to choose the most appropriate drug. Table 1 provides an evidence-based rubric, based upon the weight modulating effects of various drugs, to help decide optimal glucose-lowering treatment.
The váro-centric framework supports the recommendations of ADA/EASD and reflects the patient-centred philosophy of diabetology. It also reinforces AACE/ACE recommendations, which focus on weight control as a key factor in glycemic management. At the same time, it promotes good clinical sense by providing physicians with a simple framework upon which to base initial therapeutic strategies. The váro-centric model also highlights the synergy between patient, physician and pharmaceutical preparation. This is an unexpected literary spin off, created from the meanings of varo or város in Greek, Urban Dictionary, and Esperanto, respectively.
The váro-centric model is not complete in itself: demographic factors such as age; comorbid conditions such as endocrine and medical disease; and complications including macro- and micro-vascular dysfunction, must be taken into consideration while planning treatment. Psychosocial issues such as attitudes and ability to self-manage diabetes must be factored in. Personal and social perceptions about weight gain are also important, and should not be ignored.
With an understanding of these limitations and shortcomings, the váro-centric approach should become a globally accepted mode of clinical care in diabetology.







