Insulin, over its 95 years of existence, has revolutionized the management of diabetes. Previously limited to use in type 1 diabetes, extensive evidence supports its benefit in type 2 diabetes as well.1 In spite of this, insulin is not used as often as it should be. Multiple factors, both biomedical and psychosocial, discourage the timely initiation of insulin in real-world practice.2 This inertia delays insulin prescription, insulin acceptance, and adherence to insulin therapy. This, in turn, exposes patients to a long duration of uncontrolled glycemia, and leads to development of vascular complications.3
Extensive research and evidence describe the barriers to insulin initiation and intensification.4 These barriers have been classified as patient- and physician-related, as biomedical and psychosocial, and in terms of social marketing.5 Relatively less discussion, however, informs practice, which can be used to bridge these barriers.6
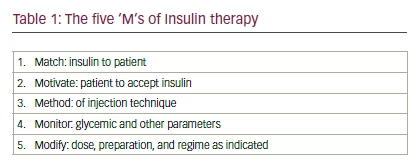
We describe the facilitators of timely insulin use as a matter of five ‘M’s (5Ms):
• match;
• motivate;
• method
• monitor; and
• modify.
The 5Ms approach conveys the need to match the patient to the appropriate insulin regime, preparation and delivery device; to motivate the patient to accept insulin through a process of informed, shared decision making; to ensure the correct method of insulin delivery by teaching injection technique; to monitor therapy by both biomedical (glycemic control, metabolic benefit) and patient reported outcomes (quality of life); and to modify therapeutic strategy, as and when needed (see Table 1).
Patient–insulin matching
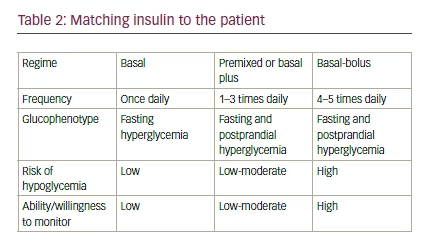
The crux of patient-centered care is to understand and respect the attitudes, wishes, and needs of the patient, while planning management. This approach, however, needs to be accompanied by respect, from the patient’s side, for biomedical issues and challenges, which the physician is better equipped to appreciate.7 Based upon a comprehensive, reciprocal understanding of each other’s viewpoints, the patient and physician can (usually) easily find an insulin regime, preparation and delivery device which suits the patient’s lifestyle, and fulfils biomedical needs as well (see Table 2).
Motivation
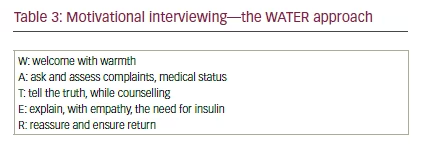
The process of finding a suitable match is not an easy or a short one. This requires a detailed two-way conversation. The physician should aim to achieve information equipoise with the patient, regarding insulin use, its benefits, risks, and costs. Simultaneously, motivation for insulin acceptance, through effective motivational interviewing, is required (see Table 3).8 This aspect of insulin prescription is also termed ‘diabetes therapy by the ear’.9 Diabetes therapy by the ear is a triptych of concepts, actions, or responsibilities. It involves listening to the patient in an empathetic manner, and responding to her or his concerns in language that is easily comprehensible. It also includes filtering of unwanted, or inappropriate information, which may reach the patient’s ears through a variety of sources and communication channels. Therapy by ear, therefore, represents use of the physician’s ears as a diagnostic tool, use of the patient’s ears as a route of administration of therapy, and enhancement of the patient’s ability to distinguish between useful and harmful health-related information that may reach her or his ears.
Method of injection
Motivation needs to be accompanied by explanation and practical demonstration of method of injection technique. Use of inappropriate or wrong technique may create unwanted complications, which hamper acceptance of insulin therapy (see Table 4). Comprehensive evidencebased guidelines are available to inform the correct injection technique.10 Insulin technique counseling needs to be incorporated in every clinic visit. Regular audits of injection sites and insulin technique helps detect local
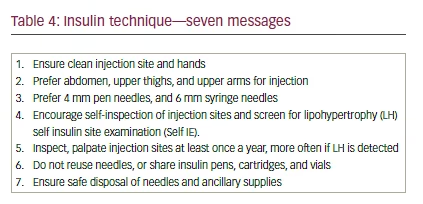
site reactions quickly, and take appropriate corrective measures, while enhancing patient confidence and satisfaction.
Monitoring
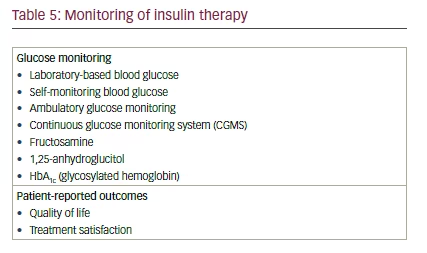
It must be noted that treatment with insulin is usually a long-term affair. A single prescription cannot (and should not) be followed indefinitely. The physician should ensure regular monitoring of glycemic parameters, listed as the glycemic pentad.11 Monitoring strategies should be decided on an individual basis (see Table 5). Monitoring techniques and frequency may vary according to the insulin regime being used, risk of hypoglycemia and glycemic variability, glycemic target, and ability of the patient to act upon monitoring data.
Modification of therapy
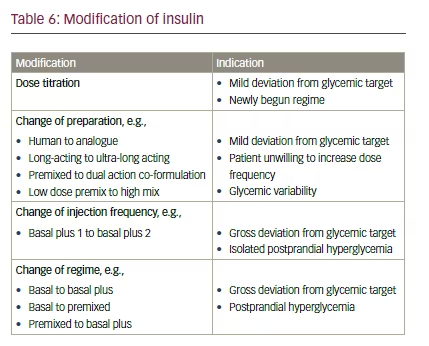
Diabetes management is a dynamic exercise, which needs regular reevaluation. Dose titration—based upon results of symptoms, glucose monitoring, and other investigations—is needed frequently. Revision of insulin regimes, and review of choice of preparations or delivery devices, may be necessary at intervals.12 Modification of dose and regime thus becomes an integral part of insulin treatment (see Table 6). Dose titration frequency is based upon patient and drug-related factors. Baseline glucose level, glycemic targets, and risk of hypoglycemia/glycemic variability influence frequency of dose titration, as does the ability of the patient or care giver to self-titrate. Drug-related factors, such as the pharmacokinetic properties of insulin preparations also impact the frequency of titration. An ultra-long-acting insulin such as degludec, for example, does not require titration before a week.13 Modification of insulin regime should be considered if one is unable to achieve targets within six to 12 weeks, or earlier if clinical circumstances indicate.
Summary
The 5Ms represent a useful pedagogic tool, which will help students of diabetology improve their skills in insulin usage. The 5Ms that matter also form a useful checklist for diabetes care professionals. This list can be used at each clinic visit to ensure that one has followed the cardinal rules of matching insulin to the patient, motivating and informing the patient about planned therapy, explaining the method of administration, monitoring health, and making appropriate modifications to treatment. In the long run, this should help encourage timely insulin prescription, acceptance, adherence and persistence. This, in turn, will improve glycemic control and prevent avoidable complications in people living with diabetes.







