COVID-19 and Endocrinology – A Bidirectional Relationship
Sanjay Kalra,1 Atul Kalhan,2 Zhanay A Akanov3
- Department of Endocrinology, Bharti Hospital, Karnal, India
- Department of Endocrinology, Royal Glamorgan Hospital, Cardiff, UK
- Kazakh Society for Study of Diabetes, Kazakhstan
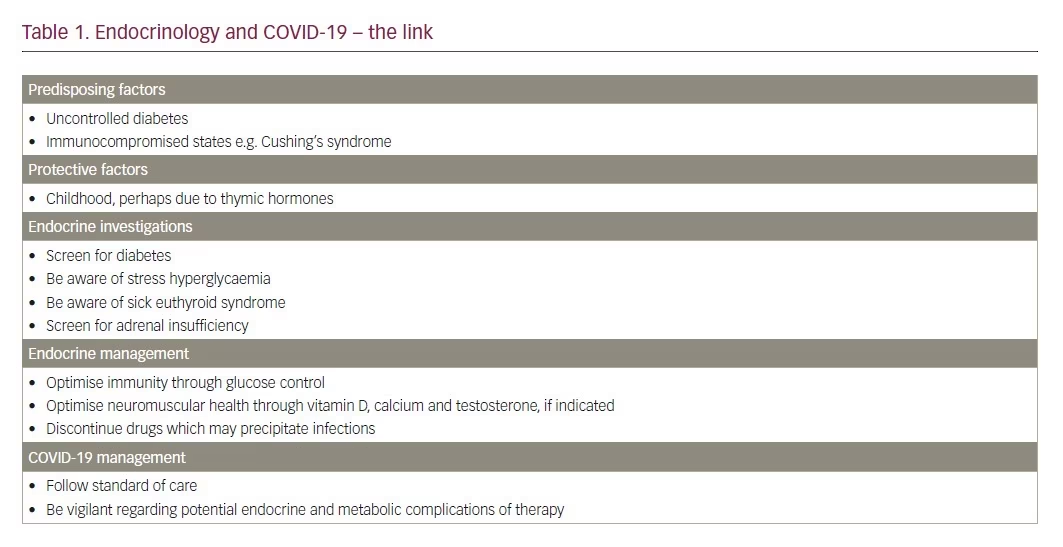
The coronavirus (COVID-19) pandemic has impacted human life in many ways. Though caused by a respiratory virus, its infection involves virtually every organ-system in the body. The endocrine system has a bidirectional relationship with the COVID-19 infection. In this article, we discuss the multifaceted endocrine implications of COVID-19 (Table 1).
Risk factors
Diabetes is one of the most important risk factors associated with mortality caused by COVID-19.1 Diabetes is known to be characterised by impaired immunity, which may lead to an increased susceptibility to COVID-19 infection, especially in those with uncontrolled glucose levels.2 Cardiovascular disease, a common comorbidity of endocrine disease including diabetes, is a significant contributor to COVID-19 morbidity.1 Though not studied, other endocrinopathies such as Cushing’s syndrome, which are characterised by immune deficiency, may be seen in those who are immunocompromised.3
Endocrine investigations
Healthcare professionals and COVID-19 management teams across the globe must be aware of the nuances of endocrine screening and diagnosis. Asymptomatic COVID-19-infected individuals should be screened for diabetes and other immunocompromised states. In the absence of other guidance, standard American Diabetes Association criteria for diagnosis of diabetes should apply.4 One must note that two abnormal glycaemic test reports are needed to confirm a diagnosis of diabetes in asymptomatic persons. As healthcare professionals should limit frequency of venesection in infected persons, random blood glucose levels may suffice for diagnosis, with glycated haemoglobin (HbA1c) if available. It seems impractical to advise a 75 g oral glucose tolerance test in those infected with COVID-19, especially in resource-constrained settings.
In those who are symptomatic, a single abnormal glucose value may suffice to diagnosis diabetes. One must be aware of the possibility of stress hyperglycaemia,5 and differentiate it from preexisting diabetes. Thyroid function tests, if ordered routinely, should be interpreted with clinical astuteness and pragmatism. COVID-19 management teams must rule out sick euthyroid syndrome prior to diagnosing de novo thyroid illness. In persons with a known history of preexisting thyroid disease, an appropriate regimen and dose titration should be performed with care.
In those with haemodynamic insufficiency, the management team may wish to order a serum cortisol, with or without stimulation, to rule out adrenal insufficiency or ‘koala bear syndrome’.7 Such a sample should be drawn prior to administering corticosteroid therapy. It is noteworthy that prednisolone, methylprednisolone and hydrocortisone all exhibit cross-reactivity with serum cortisol assays.8
Management of preexisting endocrinopathy
Most endocrinopathies are chronic in nature, and require long-term management. Those on endocrine supplementation or replacement therapy should not discontinue their medication without consulting their endocrinologist. Those who exercise regularly may need to change their routine, and shift to indoor exercises, avoiding gymnasiums and crowded outdoor spaces. Sick day rules should be valid in those at risk of, or with asymptomatic COVID-19 infection.9
Those needing hospitalisation should inform their healthcare team about their endocrine diagnosis and management. This is especially true for those with type 1 diabetes, and those with adrenal insufficiency, who need insulin and adrenal corticosteroids/mineralocorticoids for survival, respectively. Those on maintenance corticosteroid therapy must be counselled that these drugs are administered in physiologic doses, which do not cause immunosuppression.10 If patients are unable to take oral tablets, or are unfit for subcutaneous insulin, they must be given them intravenously.
Patients with hypoparathyroidism, who are on replacement vitamin D and calcium, should continue their therapy. Intravenous calcium and parenteral vitamin D/vitamin D analogues may be indicated in persons who are unable to accept enteral preparations. It must be noted that hypocalcaemia may cause weakness of chest musculature and impair breathing.11 At the same time, it may be prudent to discontinue drugs with no immediate symptomatic or metabolic benefit. Examples include medications for osteoporosis, treatment for polycystic ovary syndrome and oral contraceptives.
Diabetes management presents a special challenge, especially in those on non-insulin glucose-lowering therapy. We suggest that stable type 2 diabetes patients be counselled not to be discontinue therapy or change therapeutic regimens. Dose titration should be done as per glucose profile. Self-monitoring of blood glucose, patient-led dose titration, and telemedicine approaches should be strongly encouraged.
In those with uncontrolled hyperglycaemia, it would be pragmatic to intensify insulin dosing, rather than other oral drugs.12 A similar policy is suggested for persons who need to change their therapy, due to an inability to tolerate, or the development of contraindications to, their existing drug therapy. One must keep in mind that ancillary supplies such as insulin needles, lancets and pens must be disposed of with caution, following all biomedical waste disposal procedures.13
Basic data seem to suggest that hydroxychloroquine, which is approved for the management of type 2 diabetes in India, has antiviral properties.14 However, this does not mean that hydroxychloroquine should be considered a preferred drug for the management of diabetes complicated by COVID-19 infection. There are more effective drugs available that offer safer and better tolerated glucose control.
Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) have been implicated in adverse outcomes with COVID-19 infection.15,16 International guidelines currently state that those on these drugs should not discontinue their therapy.17 We suggest that such persons should be monitored carefully for acute kidney injury and dyselectrolytemia. We also suggest that in those with COVID-19 who need initiation, intensification or interchange of antihypertensive or anti-heart failure therapy, that ACE inhibitors, ARBs and angiotensin receptor-neprilysin inhibitors (ARNi) should be avoided. At the same time, those who need pain relief for any endocrine or metabolic conditions or complications should use paracetamol, rather thank ibuprofen or diclofenac. Opioid analgesics should be used with caution, as they may potentiate respiratory depression in high risk individuals.18
Management of COVID-19
The management of COVID-19 should proceed as per standard of care. Those with preexisting endocrinopathy, especially diabetes, present a special challenge. The utmost care should be taken to maintain euhormonal status in persons on hormonal replacement or supplementation therapy. Inadequate respiratory effort may be managed by optimising vitamin D, growth hormone or testosterone levels, as the case may be. Immune status may be bolstered by proper supplementation of insulin.
Healthcare providers should be aware of the potential endocrine and metabolic adverse effects of the drugs that they use. Corticosteroids, for example, can cause dysglycaemia, while long-term antiretroviral therapy may be associated with metabolic syndrome.19 Parenteral nutrition should be chosen with care: a balance must be maintained between calorie provision, nutrient balance and risk of dysglycaemia.
All management decisions should be guided by the principles of investigative parsimony and therapeutic parsimony.20,21 Every invasive procedure, whether blood sampling, intravenous line insertion or subcutaneous injection administration, puts a healthcare worker at risk of contracting infection. Therefore, the least required number of investigations, drugs and invasive procedures should be used, as long as they are able to achieve optimal therapeutic outcomes.
Public health management
Endocrine status can be used as a tool to triage the population for public health preventive measures. For example, those with diabetes, along with the elderly, may be asked to self-isolate or self-quarantine in view of their increased susceptibility. Similarly, those on chronic endocrine/metabolic care, such as those with hypothyroidism, metabolic bone disease or gonadal disease, may be advised to avoid routine hospital visits.22 Online/tele-consultation services may be offered to those who can avail of these. Such measures will help reduce exposure of vulnerable populations to the COVID-19 virus, and slow community spread.
An opportunity for endocrine health
The COVID-19 pandemic has brought the entire world’s focus onto health. Perhaps as never before, humankind is collectively worried about its health. Endocrinologists should take the lead in advocating endocrine hygiene, lifestyle modification and self-care, and extrapolating it to endocrine management. 23 The need for good glycaemic management, timely insulin initiation, and proper insulin technique and disposal, must be highlighted. The importance of corticosteroid replacement in persons with panhypopituitarism, and with adrenal insufficiency cannot be overstated. Similarly, the importance of good endocrine management must be explained. Healthcare providers must also be taught about the relevant nuances of endocrine screening and diagnosis.
Summary
The COVID-19 pandemic is an unfortunate development for world health. As endocrinologists, we must do our best to overcome this infection. An understanding of the various ways in which endocrine status, and endocrine interventions, influence COVID-19, and vice versa, can help improve therapeutic outcomes.
References
- Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. The Lancet. 2020;395:507–13.
- Casqueiro J, Casqueiro J, Alves C. Infections in patients with diabetes mellitus: a review of pathogenesis. Indian J Endocr Metab. 2012;16(Suppl 1):S27–S36.
- Pivonello R, Isidori AM, De Martino MC, et al. Complications of Cushing’s syndrome: state of the art. Lancet Diabetes Endocrinol. 2016;4:611–29.
- American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2020. Diabetes Care. 2020;43(Suppl 1):S14–31.
- Bar-Or D, Rael LT, Madayag RM, et al. Stress hyperglycemia in critically ill patients: insight into possible molecular pathways. Front Med. 2019;6:54.
- Ortega Chavarría MJ, Arredondo S, Daniel A, et al. Sick euthyroid syndrome. Acta Médica Grupo Ángeles. 2019;17:131–6.
- Ellger B, Debaveye Y, Van den Berghe G. Endocrine interventions in the ICU. Eur J Intern Med. 2005;16:71–82.
- El-Farhan N, Rees DA, Evans C. Measuring cortisol in serum, urine and saliva–are our assays good enough? Ann Clin Biochem. 2017;54:308–22.
- Laffel L. Sick-day management in type 1 diabetes. Endocrinol Metab Clin North Am. 2000;29:707–23.
- Bornstein SR, Allolio B, Arlt W, et al. Diagnosis and treatment of primary adrenal insufficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:364–89.
- Qin J, Deng X, Wei A, Correlation between hypocalcemia and acute exacerbation of chronic obstructive pulmonary disease in the elderly. Postgrad Med. 2019;131:319–23.
- Umpierrez GE, Pasquel FJ. Management of inpatient hyperglycemia and diabetes in older adults. Diabetes Care. 2017;40:509–17.
- Tandon N, Kalra S, Balhara YP, et al. Forum for injection technique and therapy expert recommendations, India: the Indian recommendations for best practice in insulin injection technique, 2017. Indian J Endocr Metab. 2017;21:600–17.
- Prajapat M, Sarma P, Shekhar N, et al. Drug targets for corona virus: A systematic review. Indian J Pharmacol. 2020;52:56.
- Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020:1–2.
- Singhal T. A review of coronavirus disease-2019 (COVID-19). Indian J Pediatr. 2020;87:281–6.
- Position Statement of the ESC Council on Hypertension on ACE-Inhibitors and Angiotensin Receptor Blockers. Available at: escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang. (accessed 19 March 2020).
- Balhara YPS, Kalra S, Singh S. Pragmatic opioid use in painful diabetic neuropathy. Eur Endocrinol. 2020;16: Epub ahead of print.
- Yi D, Kang YH. Drug-induced diabetes mellitus. J Korean Diabetes. 2017;18:160–8.
- Kalra S, Saboo B. The law of investigative parsimony. J Pak Med Assoc. 2018;68:817–8.
- Kalra S, Gupta Y, Sahay R. The law of therapeutic parsimony. Indian J Endocr Metab. 2016 1;20:283–5.
- COVID-19 outbreak: guidance for people with diabetes. Available at: idf.org/our-network/regions-members/europe/europe-news/196-information-on-corona-virus-disease-2019-covid-19-outbreak-and-guidance-for-people-with-diabetes.html (accessed 19 March 2020).
- Kalra S, Gupta Y, Sahay R. Endocrine hygiene. Indian J Endocr Metab. 2016;20:134–6.
Support: Commissioned, edited and funded by Touch Medical Media
Published: 30 March 2020




