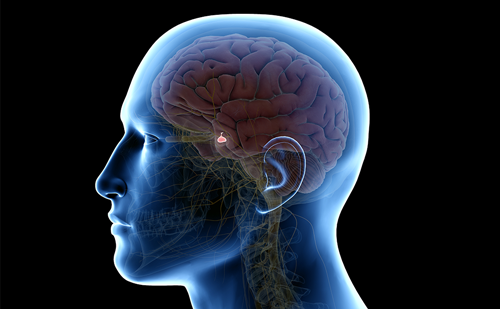
Example of myth: pituitary tumors are rare.
Fact: these tumors are very common and can be detected in nearly 17.6% of the population (see description of meta-analysis below).
Example: the tumor is so small, it is best to watch it and wait.
Example of myth: pituitary tumors are rare.
Fact: these tumors are very common and can be detected in nearly 17.6% of the population (see description of meta-analysis below).
Example: the tumor is so small, it is best to watch it and wait.
Fact: size of the tumor may have little relevance to the damage it can wreak on the patients.About 40% of the type of pituitary tumor that causes Cushing’s syndrome or excess of the steroid hormone cortisol are too small to be seen on magnetic resonance imaging (MRI), while about 30% of Prolactin secreting tumors are also too small to be seen.
The suffering of the patient and the many insidious symptoms and disorders progressing with the patient’s discomfort are met with shrugged shoulders by too many physicians who still believe an MRI is the ‘gold standard’ for diagnosis.
Example: a computed tomography (CT) scan or an MRI shows nothing and the physician declares the patient free of clinically significant symptoms from an endocrine point of view.
Fact: a well qualified pituitary endocrinologist basically diagnoses in five different ways, as follows:
- a complete medical history/examination/probing questions;
- blood samples;
- urine samples;
- salivary samples; and
- a visual field test.
The MRI is ideally used to discern the tumors direction of growth, size, invasiveness, etc., confirming what the experienced clinician had already suspected based on their tests and examination.
Example: acromegaly can be ruled out; the patient does not ‘look’ acromegalic; or, the patient does not have Cushingoid features.
Fact: no one ‘looks’ acromegalic—only many years of misdiagnosis or very advanced disease allows a patient to change so profoundly as to become disfigured sufficiently to make them un-recognizable to childhood friends or distant family members.The same holds true for Cushing’s disease. The weight gain, stretch marks, or ‘buffalo hump’ only become apparent because the patient goes undiagnosed for a long (often years) period of time.
In a remarkably high number of patients, however, it has become clear that the previously relied upon ‘visual markers’ for diagnosing both Cushing’s disease and acromegaly are neither reliable nor sensitive enough to identify these disorders. Again, while a number of biochemical and imaging technologies have developed,the methods of applying these techniques are lagging behind significantly. Conversely, many imaging studies, applied for other purposes, are identifying far too many incidental findings. It should be pointed out that there are a great number of tumor (adenoma) types currently identified, as well as hormonal disorders that may or may not be tumor-related. Some of the more common pituitary/hormonal tumor/cyst/lesion/disorders are outlined below. The relative percentages of hormonal production identified by immunohistochemistry breakdown are as follows:
- prolactin (PRL), 43% of the patient community;
- 4.9% for adrenocorticotrophic hormone (ACTH) Cushing’s disease);
- 2.8% for growth hormone (GH); and
- 0.7% for thyroid secreting hormone (TSH).
The balance is generally the group of the so-called nonfunctioning adenomas that do not secrete an excess of hormones. These figures do not include the craniopharyngiomas, Rathke’s cleft cyst, or arachnoid cysts that also do not secrete any hormones but frequently impair the ability of the normal gland to secrete hormones rendering patients hypopituitary. On the surface, many such patients are diagnosed as low on thyroid hormone or testosterone and supplemented without true identification of the underlying cause. An arachnoid cyst, for instance, can have a multitude of symptoms that are often not understood by clinicians who frequently ascribe weight gain, gun-shot noises in the head, inappropriate lactation, mental and emotional disorders/disturbances, cognitive disorders, migraine headaches, etc. to ‘nerves’, hypochondria, or unknown causes. All too often, these patients are denied the opportunity of receiving a specific diagnosis and treatment plan.
A meta-analysis sponsored by the Pituitary Network Association beginning in 2001 and published by the American Cancer Society in June 2004 articulates many of these concerns. This meta-analysis, based on 13 independent studies, estimated the prevalence rate of pituitary adenomas to be 16.7%. Separate analyses of autopsy and radiographic data produced estimated prevalence rates of 14.4% and 22.5%, respectively.These figures indicate that pituitary tumors are fairly common in the general population.Tumors measuring in excess of 10mm in diameter were estimated to occur at a rate of one in 600 persons. Epidemiologic, autopsy, and radiographic studies have been used to estimate the prevalence of pituitary adenomas; however, epidemiologic studies are limited by their dependence on population-specific registries, which subject them to bias from regional influences such as diagnostic practices, reporting patterns, and case definitions. Moreover, the clinical usefulness of epidemiologic studies is limited because their dependence on clinical diagnosis to identify pituitary adenomas results in the exclusion of silent or incidental tumors from analysis. Although generally considered benign, these adenomas can have considerable compressive mass effects, endocrine manifestations with serious morbidity, or both. In contrast to epidemiologic studies, autopsy and radiographic studies are not registry-dependent; therefore, they avoid population bias by selecting subjects from across regions.Thus, to determine an accurate estimate of the prevalence of pituitary adenomas based on a broad cross-section of the population, the following analysis was based on both autopsy and radiographic studies using CT or MRI.The study found prolactinomas to be the most common form of pituitary adenoma. This is consistent with earlier findings by Burrow et al. that documented premortem serum prolactin concentrations and showed them to be higher in patients in whom prolactinomas were identified at post mortem. This is an important observation because it provides evidence that the high prevalence of small adenomas observed in many studies may be clinically relevant. It is widely appreciated, for example, that modest elevations of PRL concentration have the potential to result in hypogonadism. This can result in symptoms of diminished libido, potency, and fertility in both men and women.
It is common to consider small, incidentally discovered lesions in the pituitary gland clinically insignificant. However, multiple lines of evidence indicate that small lesions within the pituitary gland may be clinically significant. For example, sensitive MRI techniques do not detect demonstrable tumors in approximately 40% of patients with Cushing’s disease, a well recognized condition with serious co-morbidities. Moreover, hypopituitarism, or loss of normal pituitary function, has recently been reported to occur at an estimated frequency of 4.21 cases/100,000 in the absence of large pituitary lesions, further underscoring the potential for functional relevance of small pituitary lesions.