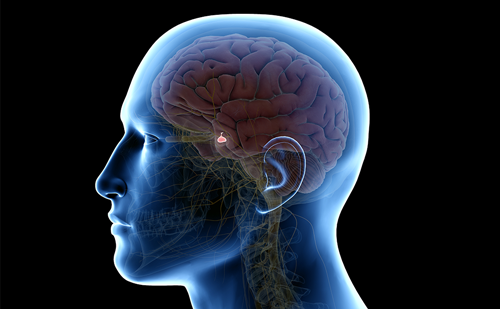
Acromegaly is a rare disease due to growth hormone (GH) hypersecretion by a pituitary adenoma. The rheumatologic, cardiovascular, respiratory and metabolic consequences determine the prognosis, and their severity increases with the length and degree of GH hypersecretion. The prognosis of acromegaly also depends on the culprit pituitary tumor, which may cause a tumoral syndrome, with headache and/or visual disorders due to optic chiasm compression.
Prognosis of Acromegaly
Acromegaly is a rare disease due to growth hormone (GH) hypersecretion by a pituitary adenoma. The rheumatologic, cardiovascular, respiratory and metabolic consequences determine the prognosis, and their severity increases with the length and degree of GH hypersecretion. The prognosis of acromegaly also depends on the culprit pituitary tumor, which may cause a tumoral syndrome, with headache and/or visual disorders due to optic chiasm compression.
Prognosis of Acromegaly
When untreated, acromegalic patients have a 10-year life expectancy reduction, particularly due to cardiovascular and respiratory problems and to the increased risk of neoplasms. Standardized mortality ratio, SMR is from 1.2 to 3.3 in recent series. The most important predictive factor of mortality is the so-called “final” post-therapeutic GH level. When <2.5 μg/L, SMR is non-significantly different from that of the general population, while it is between 1.4 and 2 when > 2.5 μg/L. Only one recent study demonstrated a significant trend for increased mortality when GH levels exceed 1μg/l. Few studies have provided any support for the use of IGF1 as a marker for long term outcome. This was not confirmed by others.
Treatment Objectives
The clinical aims are to relieve symptoms, to reduce the volume of the pituitary tumor, to avoid its tumor relapse, and to improve long-term morbidity and mortality. Recent epidemiological studies helped to refine the definitions of “cure” and good disease control, which are now far more precise: in a recent consensus statement, criteria for cure of acromegaly were defined as achieving a GH level of less than 1μg/l during OGTT and normal age-related serum IGF1 level.
A Stepwise Therapeutic Strategy
Surgery (usually by the trans-sphenoidal route) is the classical first-line treatment. Tumor excision normalizes GH and IGF-I concentrations in only 40 to 70% of cases, depending on the size of the tumor (microadenomas are more amenable to cure), preoperative GH concentrations (the success rate is higher when preoperative GH concentrations are lower), and the surgeon’s experience.
Before the era of medical treatment, radiotherapy was used in second line, when surgery has failed to achieve control of GH/IGF-1 hypersecretion. Fractioned irradiation delivering a total dose of 45 to 50 Gy, yields GH concentrations below 2 μg/l and normal IGF-I levels in 5 to 60% of patients, after a median follow-up of about 7 years. In studies with longer follow-up, fractionated radiotherapy normalizes the IGF-I level in more than 70% of patients beyond 10 years. Baseline GH concentration seems to be predictive of treatment outcome. However, radiotherapy leads to variable degrees of hypopituitarism in 80 to 100% of patients after 10-15 years. Complications such as radionecrosis and optic neuropathy are now rare. In contrast, the risk of stroke may be increased, sometimes many years after irradiation. When the lesions are small and located at least 5 mm from the optic chiasma, stereotactic irradiation (e.g. using a gamma-knife) is interesting. According to a recent French study, efficacy seems similar to that of fractionated radiotherapy. Indeed, less than 20% of patients have normal IGF-I levels and GH < 2 μg/l an average of 4 years after the procedure.
As surgical treatment even combined with radiotherapy is not able to control GH/IGF-I GH levels in all patients with acromegaly, a medical alternative is useful in order to achieve the recommended criteria of control of the disease and to decrease the morbidity and the mortality associated with acromegaly
Medical Treatment
Three types of drugs are currently available
- Bromocriptine and other dopamine agonists such as cabergoline are able to improve symptoms of acromegaly in few patients and to decrease GH secretion.
- Somatostatin analogs (SA). Somatostatin, the hypothalamic GH-release inhibitory native peptide had a too short half-life to be administered easily. The first synthesized SA, octreotide, is an octapeptide with a prolonged half-life and an increased potency and is available since more than 20 years. Given initially subcutaneously (100 to 500 μg) three times daily, it rapidly proved to be able to control GH hypersecretion in a significant proportion of patients. A long-acting form (by encapsulation in microspheres) has subsequently been proposed allowing once-monthly intramuscular injections (10, 20 or 30 mg) with the same efficacy. More than 10 years ago, another SA, named lanreotide (also an octapeptide) was also proposed. Initially it has also been encapsulated in microspheres allowing a prolonged release for twice or thrice-monthly intramuscular 30 mg injections, and proved to be effective in acromegaly. Recently a sursaturated lanreotide solution (lanreotide Autogel®) which forms a gel allowing slow release and enabling a once-monthly administration (60, 90 or 120 mg) as a deep sub-cutaneous injection has been developed. Somatostatin and SAs bind to somatostatin receptors (sst) present on the cell surface of target organs. Five subtypes (1 to 5) have been described. The current available SAs bind with high affinity to sst2 and 5. As a significant percentage of GH-secreting adenomas seem partially or totally resistant to octreotide or lanreotide, due in part to a variable tumoral expression or reduced receptor density of the five known sst there is a place for the development of new somatostatin analogues, more potent and with enhanced binding capacity to some sst. SOM230, a novel analog displaying high-affinity binding to human sst1, 2, 3 and 5 is a potent inhibitor of GH and IGF1 in vitro and in several animal models. Due to heterogeneous expression of sst2 and 5 in GH-secreting tumors, a bispecific SA, such as BIM-23244 that can activate both receptors could achieve better control of GH hypersecretion in a larger number of acromegalic patients. Combination of dopamine agonists and SA may be beneficial for some patients but long-term studies assessing this therapeutic association are not currently available. Researchers are working on dopastatins which are chimeric drugs able to bind to dopamine and to somatostatin receptors which may produce a synergistic effect on GH secretion. Side-effects of SA are benign: digestive problems are minor and most often transitory (abdominal cramps, diarrhea, flatulence); cholelithiasis occur in 10 to 55 %, are generally asymptomatic and must be treated conservatively; despite reduction in insulin secretion due to SA, glucose tolerance alterations are generally of minor significance.
- Pegvisomant, is a recently developed antagonist of GH receptor (GH-R) which blocks the effects of GH at the level of its target organs. It was obtained by combining mutagenesis of GH gene: a substitution of eight amino acids in the binding site 1 of a molecule of GH, resulting in an increased affinity for the GH-R and a mutation in binding site 2, rendering ineffective the binding to the second molecule of GH-R and therefore blocking the GH-R dimerization and the intracellular GH signalling. To enhance its half-life, several polyethylene glycol (PEG) molecules were added to the molecule. Pegvisomant has proved to be effective in lowering IGF-I; however, GH concentrations increase and efficacy must only be regarded on IGF-I levels. The drug is administered once-daily, by subcutaneous injection, at a dose of 10, 15 or 20 mg. Side-effects are limited to hepatitis, justifying follow-up of liver function every month during the first six months. There is uncertainity about the effects of the drug on tumoral volume, some rare patients displaying an increase volume during treatment with pegvisomant : this may be the consequence of the loose of negative feed-back of IGF-I on somatotrophs or, alternatively to the natural history of the adenoma in some of the patients. A close surveillance of tumoral volume during treatment with pegvisomant is thus recommended.
Results of the Various Treatments
- Bromocriptine or other dopaminergic agonists produce improvement in clinical symptoms of acromegaly in half of the patients, substantially decrease GH levels in some patients. A review of 31 published studies of bromocriptine involving 549 patients with acromegaly demonstrated very modest results: suppression of GH less than 5μg/l in 20% of cases and normalization of IGF-I levels in less than 10 % of cases. Better results seem to be obtained with cabergoline: near 40% of acromegalic patients were reported to normalized their IGF-I levels in a multicenter study from Belgium.
- Treatment with somatostatin-analogs has now gained a wide place in the medical treatment of a acromegaly.
Antisecretory Effects
GH levels are decreased in 50-80 % of patients treated with octreotide subcutaneously three times daily. Up to 50 % of acromegalic patients may be considered as “controlled” (GH plasma levels less than 2 μg/L [20-30%] and/or normal IGF-I [20-60%]) with this treatment.
Similar results are obtained with lanreotide LAR 30 mg administered intramuscularly every 10 or 14 days (GH plasma levels less than 2 μg/L [30-70%] and/or normal IGFI [40-70%]) or with octreotide LAR given im every month at the dose of 10-30 mg (GH plasma levels less than 2 μg/L [50-60%] and/or normal IGF1 [60-90%]). Lanreotide Autogel” (60, 90 and 120mg) is at least as effective and well-tolerated as lanreotide PR 30mg injected every 7-14 days.
The various figures obtained between studies are probably explained by the variation in the method used for IGFI assay, and by the differences in the inclusion criteria chosen in each study. Indeed, in some of the studies, patients were included if they were previously demonstrated to be responsive to octreotide SC, while in others, patients were entered blindly.
Freda et al. performed recently a meta-analysis on the effects of long-acting SA therapy in acromegaly. They found that, among subjects not selected for SA responsiveness before study entry, both GH efficacy criteria and IGF-I normalization were met in a greater proportion of those treated with octreotide LAR vs. lanreotide SR. (54 and 63% vs. 48 and 42%, respectively).
It has long been claimed that the efficacy of octreotide sc or LAR or lanreotide LP as primary treatment (in de novo patients) was equivalent to that of secondary treatment (in patients previously treated with surgery and/or radiotherapy). In fact, according to the meta-analysis of Freda et al., IGF-I normalization occurred in a greater proportion of secondary octreotide LAR- vs. primary octreotide-treated subjects.
Different long term studies have shown that biochemical cure under long acting SA seems to improve with time.
Antitumoral Effect
Clinically significant tumor shrinkage has been seen in a number of studies, particularly in patients undergoing primary medical therapy whether with octreotide sc, octreotide LAR or lanreotide SR (rev in. A meta-analysis of all the published studies involving de novo patients treated with long acting SA, showed that a ~50% decrease in pituitary mass is achieved. Importantly, the initial pre-treatment tumor size is a determinant of the significance of measured shrinkage. Fourteen studies provided a definition of tumor shrinkage and described the percentage of patients that demonstrated a significant shrinkage in tumor size when used as primary treatment. As a whole, 36.6 % of the patients had a significant decrease in tumor size. The mean reduction was 19.4%. The percentage of patients demonstrating tumor size reduction while receiving short-acting octreotide seems to be not different from the percentage of patients receiving long-acting preparations.
Except for one study, persistent tumor growth has generally not been observed in patients receiving SA therapy. When SA are discontinued, tumor regrowth appears to occur within 6 month. In a review of 36 studies involving 921 patients, only 3 studies reported tumor growth during SA treatment. In these studies, tumor growth was observed either in cases of invasive, « resistant » tumors, in patients treated with lanreotide 30 mg after a short-term (1-month) treatment or due to the cystic transformation of a tumor. Thus, with long acting treatment, tumor growth is controlled in >97% of patients.
Preoperative somatostatin analog treatment is able to improve the patient’s general condition before pituitary surgery. Some authors also advocate its use for improving surgical remission rates by allowing the tumor to shrink and facilitate a more complete resection. In fact, this question remains controversial : some series have reported a beneficial effect while others did not. Nevertheless when an improvement in surgical outcome is noted, it seems to be limited to intrasellar non-invasive macroadenomas).
In patients with large invasive tumors, treated primarily with SA and in whom medical treatment with SA is unable to achieve good GH/IGF-I control, it may be interesting to propose a surgical tumor debulking and to re-introduce SA treatment. This may allow to increase the likelihood of achieving biochemical disease control under SA.
Perspectives
In a recent study, administration of a single dose of 100 and 250μg SOM230 was compared to 100 μg octreotide. Some patients showed similar efficacy of both drugs on GH levels, whereas in others SOM230 was either more or less effective, as compared with octreotide. This may be related to its additionnal suppressive effect on GH secretion via sst5. At the present time, there are now human studies with the bispecific SA BIM2344 or with dopastatines.
Treatment with the GH-receptor antagonist pegvisomant, has proved to be effective in the control of clinical symptoms of acromegaly and allows normalization of IGF-I levels in the great majority of patients. In a randomized double-blind placebo controlled trial during 12 weeks, in 112 patients, at a dose of 10, 15, 20 mg/d, normal IGF1 levels were achieved in 89% of patients with high dose of pegvisomant (20mg/d sc). In a study collecting all the data obtained with this drug, normalization of serum IGF1 levels was observed in 97% of 90 patients for more than 12 months, using doses of up to 40mg. While treatment with SA may be responsible for a worsening of glucose tolerance (due to its suppressive effects on insulin secretion), pegvisomant, by acting only on insulin resistance (which is improved in parallel with the reduction of IGF-I levels) and not on insulin secretion does not impair glucose tolerance and may thus be recommended in acromegalic patients with diabetes or IGT. Van der Lely et al. reported non significant alteration in mean tumor volume. However tumor growth was observed in few patients. Interestingly, in one of them cotreatment with octreotide halted further tumor growth and induced a synergic decrease in serum IGF1 concentration. Recently, an association of SA (octreotide LAR once monthly) and pegvisomant (administered weekly at a dose of 60 mg on average) was shown to normalize IGF-I in 18 of 19 (95%) patients whose acromegaly was resistant to SA administered alone. This combined treatment is effective, might increase compliance, and could greatly reduce the costs of medical treatment for acromegaly in some patients.
Recommendations for Treatment of Acromegaly
The proposed management of patients with acromegaly (which grossly corresponds to the recommendations of a recent consensus meeting on medical treatment of acromegaly is given on Figure 1.
- Trans-sphenoidal surgery is generally the first-line therapy. In selected patients, either if surgery is contra-indicated (e.g. compromised cardiac or respiratory function) or if the probability of surgical cure is low (e.g. in patients with very large and/or invasive tumors), SA may be a reasonable primary therapeutic modality provided that the tumor does not threaten vision or neurological function.
- After surgery a biochemical evaluation (GH and IGF-I) allows to know if the disease is controlled or not. In case of persisting disease, SA are generally prescribed as a second-line treatment (eventually preceeded by a trial of dopamine agonists, particularly cabergoline).
- If the disease is controlled under SA, regular assessment (both biochemical and on tumoral volume) is necessary.
- In case of persistent disease despite SA treatment, some patients may be reoperated, in particular for debulking a residual tumor before a novel trial of SA treatment. Otherwise, there is an indication for third-line treatment which may be either radiotherapy or GH antagonist (pegvisomant).
- Postoperative radiation therapy (50 to 55 Gy) is performed for partially resected tumors or when GH levels remain elevated. SA are generally given in waiting for the delayed effects of radiation therapy.
- However, due to the potential side-effects of radiotherapy, we generally prefer to delay radiation therapy and to first switch patients from SA therapy to pegvisomant if there is no concern with tumor mass. If there is a concern with tumor mass, pegvisomant may be associated with SA.
- During treatment with pegvisomant, a close monitoring of IGF-I (for evaluating acromegaly control) and tumor mass is recommended, in order to diagnose a potential increase in tumor volume which may necessitate surgery and/or radiotherapy.
■
A version of this article containing references can be found in the Reference Section on the website supporting this briefing (www.touchbriefings.com).