Cushing’s disease is caused by a pituitary adenoma that secretes elevated levels of adrenocorticotropic hormone (ACTH), which stimulates the adrenal glands to produce excess cortisol.1 The tumours are most frequently microadenomas (≤1 cm in diameter) while corticotroph macroadenomas are responsible for approximately 10 % of cases.
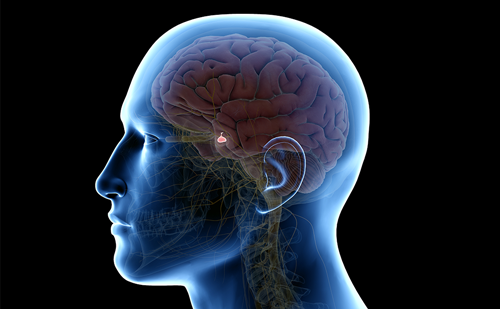
Cushing’s disease is caused by a pituitary adenoma that secretes elevated levels of adrenocorticotropic hormone (ACTH), which stimulates the adrenal glands to produce excess cortisol.1 The tumours are most frequently microadenomas (≤1 cm in diameter) while corticotroph macroadenomas are responsible for approximately 10 % of cases. Cushing’s disease is the most common form of endogenous Cushing’s syndrome accounting for about 70 % of patients with this condition and has an estimated annual incidence of 0.1–2.0 new cases per 100,000 worldwide.2–4 Chronic stimulation by ACTH produces diffuse bilateral hyperplasia of the adrenal cortex which can sometimes become nodular and enlarged. The primary clinical symptoms of Cushing’s disease are due to hypercortisolism. Symptoms and signs develop gradually and include weight gain (particularly on the trunk and face), fatigue, proximal muscle weakness, oedema, diabetes, hypertension, sleep disturbances, cognitive impairment, depression, osteoporosis, infections, skin atrophy, ecchymosis, hirsutism and menstrual irregularities in women and decreased libido and erectile dysfunction in men. If Cushing’s disease is left untreated or uncontrolled, this can result in severe complications including ischaemic and thromboembolic cardiovascular events.5 Individuals with such progression have a mortality rate four to five times higher than an age- and sex-matched population.4,6,7
Surgical Therapy of Cushing’s Disease
The treatment goals in Cushing’s disease include elective removal of corticotroph tumour while preserving pituitary function, reversal of clinical features, normalisation of biochemical changes and long-term control without recurrence. Surgical removal of the tumour is the first-line treatment; however, the risk of initial surgical failure in microadenoma is 10–35 % and recurrence of Cushing’s disease may reach 20 % in the subsequent ten years. In the case of macroadenoma, surgery is unsuccessful in achieving remission in >45 % of cases, remission rates are lower (12–45 %) and recurrence occurs sooner than in microadenoma (mean 16 versus 49 months).8 The reported rates of remission vary as a result of differing criteria of cortisol values and endpoints used to determine remission, and differences in the timeframe of patient monitoring (see Table 1). Patil et al. found that although surgical remission was achieved in 85.6 % of 215 patients with Cushing’s disease who underwent first line transsphenoidal surgery for resection of a pituitary microadenoma, disease recurrence was found in a quarter of these (25.5 %) at five-year follow up.9 Another study reported a remission rate of 56 % of 63 patients at 9.6 years post-transsphenoidal surgery.10
To view the full article in PDF or eBook formats, please click on the icons above.