In 1962, Dr Jacqueline Noonan presented at the Midwest Pediatric Research Meeting a clinical study on associated non-cardiac anomalies in children with congenital heart disease, in which nine patients—six males and three females—with distinctive facies and pulmonary stenosis were identified.6 The facies were remarkably similar and included hypertelorism, a relatively short neck, low-set posteriorly rotated ears, a slight antimongoloid slant to the eyes, micrognathia, ptosis, and, often, curly hair. The majority were of small stature, exhibiting a significant chest deformity.
In 1962, Dr Jacqueline Noonan presented at the Midwest Pediatric Research Meeting a clinical study on associated non-cardiac anomalies in children with congenital heart disease, in which nine patients—six males and three females—with distinctive facies and pulmonary stenosis were identified.6 The facies were remarkably similar and included hypertelorism, a relatively short neck, low-set posteriorly rotated ears, a slight antimongoloid slant to the eyes, micrognathia, ptosis, and, often, curly hair. The majority were of small stature, exhibiting a significant chest deformity. Many males had one or both testes undescended and delayed puberty. Noonan felt these patients represented a new syndrome that was distinctive from the previously described Turner syndrome. In 1968, research on these nine and an additional 10 patients (12 males and seven females) were published, outlining further findings of congenital heart defects, hypotonia, hepatosplenomegaly, scoliosis, a duplicated right kidney, and a variety of skin manifestations such as pigmented moles or nevi.7 As Noonan was the first to describe this clinically and genetically heterogeneic condition affecting both sexes, Dr John Opitz proposed the eponym Noonan syndrome.8
Clinical Findings
Noonan syndrome is one of the most common non-chromosomal disorders found in children with congenital heart disease, occurring worldwide with an estimated incidence of between 1:1,000 and 1:2,500.9 With complete penetrance but variable expressivity, the phenotype of this autosomal dominant disorder ranges from mild (often unrecognized and undiagnosed) to severe (diagnosis possible at birth). In addition to the wide phenotypic variation in Noonan syndrome, the phenotype of the Noonan syndrome patient also changes with age.10 Noonan syndrome is difficult to diagnose in the newborn by facial appearance alone. The forehead is often sloping and broad, and the ears may be thick and posteriorly rotated. Apparent ocular hypertelorism and antimongoloid slant of the palpebral fissures, a deep philtrum, and mild retrognathia may also be present. However, the presence of excess nuchal skin, indicative of pre-natal cystic hygroma, can assist in the diagnosis of Noonan syndrome. From neonate to two years of age, the head often appears relatively large. The malar eminences are flat and the eyes are prominent and round. The nasal bridge is depressed, and the neck appears short but is no longer webbed. By 24–36 months, the body appears stockier, allowing the chest deformities to become more pronounced. In childhood, facial features are coarse, and the chin lengthens to yield a more triangular face (see Figures 1 and 2). The eyes become less prominent, and ptosis may become more apparent. The low hairline and webbing may become more obvious as the neck elongates. The triangular facial features become even sharper in teenagers and young adults, with a pinched root and a thin, high bridge on the nose. Older adults exhibit prominent nasal labial folds, a high anterior hairline, and a transparent and wrinkled appearance to the skin (see Figure 3).
The majority of patients with Noonan syndrome have an unremarkable pre-natal history, but polyhydramnios, cystic hygroma, and fetal hydrops are commonly reported.11,12 Cystic hygromas are often discovered by use of fetal ultrasound in early pregnancy in fetuses that subsequently show signs of Noonan syndrome, which regress or disappear late in the second trimester.13 However suggestive, none of these findings is specific for Noonan syndrome. Furthermore, Noonan syndrome is not generally suspected in the neonatal period if the newborn does not exhibit any edema. Although overt edema is not common, many infants afflicted with Noonan syndrome lose a substantial amount of weight during the first week of life, suggestive of some degree of fetal edema. Despite a normal appearance at birth, and height and weight within the normal limits, height growth slows within a few months of age; over 70% of individuals with Noonan syndrome are of significantly short stature, falling below the third percentile of height.14 Feeding difficulties in early infancy often lead to hospitalization owing to lethargy, poor feeding, vomiting, and possible sepsis or failure to thrive.15 The cause of this poor feeding is not well understood, but some patients have gastroesophageal reflux and a few cases of intestinal malrotation and immature co-ordination of gastrointestinal musculature have been reported.16 Noonan syndrome should be suspected in any infant appearing dysmorphic with some hypotonia, poor feeding, and failure to thrive for no apparent cause.
Over 90% of patients with Noonan syndrome have a pectus carinatum or pectus excavatum resulting in a shield-like chest deformity. An abnormal spinal curvature (scoliosis), hunchback (kyphosis), or clubfoot (talipes equinovarus) is present in 10–15% of patients.17 Many have hyperextensible joints and muscle hypotonia is common, although hypotonia generally improves with time. Patients with Noonan syndrome have reported poor co-ordination; this is attributed to strabismus, visual problems such as ocular refractive errors, and muscular hyptonia, which can account for mild motor delays. Conductive hearing loss is also fairly frequent. It is recommended that all children with Noonan syndrome undergo a hearing evaluation and eye examination. Infants with Noonan syndrome generally exhibit slower development: sitting is often delayed until about 10 months of age, and walking and talking occur closer to two and 2.5 years of age, respectively. True mental retardation is not common, and although learning disabilities are frequent, the overall intelligence quotient (IQ) of patients with Noonan syndrome is about 10 points lower than the mean; however, IQs up to 130 have been reported.18,19 Most patients graduate from high school and college, and achievement of PhD degrees have been reported.20 Seizures are not particularly common, but have been reported in 13% of patients.15 Unexplained peripheral neuropathy has also been observed. Other neurological complications have included spina bifida occulta, subarachnoid hemorrhage from aneurysm, and syringomyelia.17 Arnold- Chiari malformation has also been reported in a number of patients with Noonan syndrome, and may warrant surgery if it becomes symptomatic.21
Hepatosplenomegaly, often unexplained, is present in approximately 25% of patients with Noonan syndrome. Reports of bleeding problems and easy bruising are also frequent. In 1983, Kitchens described a common association with factor XI deficiency;22 deficiencies of factor VIII and XII, thrombocytopenia, and platelet dysfunction have since been described.23,24 Prothrombin time, partial thromboplastin time, bleeding time, and platelet counts should be obtained and aspirin or aspirincontaining products avoided if bleeding problems are suspected. The occurrence of juvenile myelomonocytic leukemia (JMML) in patients with Noonan syndrome has previously been reported;25 it is not clear whether individuals with Noonan syndrome are at an increased risk for other malignancies. Lymphatic problems occur in an estimated 20% of patients, and may present serious problems. Chylous effusion following surgery is a known risk in these patients. Chylothorax can also arise spontaneously and can be fatal in newborns, as the condition is poorly understood and difficult to manage. Both intestinal lymphangiectasia and pulmonary lymphangiectasia have been reported, but are quite rare.26,27
Cardiac Findings
Cardiac abnormalities are present in over 80% of patients with Noonan syndrome,15,28–30 with pulmonary stenosis being the most frequently observed cardiac lesion. The pulmonary valve may be only mildly dysplastic with no significant obstruction; for these patients, the long-term prognosis is excellent. Unlike non-syndromic pulmonary stenosis, in which progression is not usually observed past two years of age, some patients with Noonan syndrome may experience a rapid progression of valvular obstruction. If obstruction is significant, the patient may require surgery. Atrial septal defects and pulmonary artery branch stenosis frequently accompany pulmonary valve stenosis. Fortunately, many children will have only mild pulmonary stenosis with no intervention required.
Ostium primum atrial defects, ventricular septal defects, and anomalous pulmonary venous return have also been reported. Although right-sided cardiac lesions predominate, left-sided lesions such as valvar aortic stenosis, subaortic stenosis, supravalvar aortic stenosis, coarctation of the aorta, and patent ductus arteriosus also occur. Except for transposition of the great arteries, nearly every kind of heart disease has been described in Noonan syndrome.
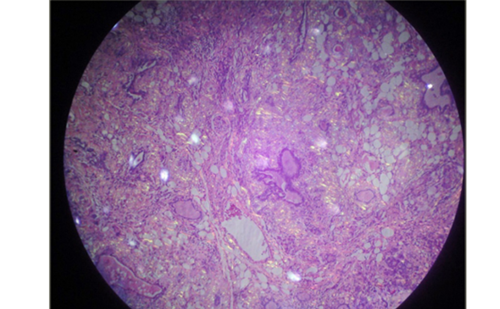
Hypertrophic cardiomyopathy was first described in Noonan syndrome by Ehlers et al. in 1972,31 and occurs in about 20% of patients with Noonan syndrome. The condition is poorly understood, with marked variability in course and prognosis. Similar to non-syndromic familial hypertrophic cardiomyopathy, hypertrophic cardiomyopathy affiliated with Noonan syndrome shows myocardial disarray and thick-walled intramural coronary arteries. Hypertrophic cardiomyopathy can be symptomatic and rapidly progressive in infancy in some patients, or remain asymptomatic, or develop later in life in other patients. Symptomatic hypertrophic cardiomyopathy in Noonan syndrome is significantly associated with mortality in infancy.28,29 Hypertrophic cardiomyopathy can be treated with beta-blockers, calcium channel blockers, and, if severely obstructed, surgical myomectomy. All children with Noonan syndrome should be seen by a pediatric cardiologist and have a cardiac ultrasound. Periodic re-evaluation is important as cardiac findings may change and/or develop over time. Genetics of Noonan Syndrome
Phenotypic similarities between Noonan syndrome and Turner syndrome led investigators to look for linkage to the X chromosome, but none was ever found.32 In 1994, Jamieson et al. performed a linkage analysis on two multigenerational families and mapped the gene for Noonan syndrome to the distal part of chromosome 12q (12q22-qter).33 As not all families in the study exhibited this linkage, additional genes were likely to be involved in the etiology of Noonan syndrome. In 2001, Tartaglia et al found a mutation in the PTPN11 gene on chromosome 12 that was present in approximately 50% of patients with Noonan syndrome.34 The SHP-2 protein, a product of PTPN11, is essential in several intracellular signal transduction pathways, including the Ras-mitogen activated protein kinase (RAS-MAPK) pathway, which is involved in cell proliferation, differentiation, survival, and apoptosis. SHP-2 also controls a number of developmental processes including cardiac semilunar valvulargenesis.
Genotype–phenotype studies have shown a great variability in the mutations occurring in PTPN11, with the majority located in exons 3, 8, and 13. While over 80% of patients with a mutation in PTPN11 have congenital heart disease and pulmonary stenosis presents more frequently in patients with a mutation (50–80%) than in those without, the incidence of hypertrophic cardiomyopathy was lower in patients with a mutation (0–10%) compared with those without (20–30%).34–39 Mutations in three additional genes have been identified in Noonan syndrome in the past three years: KRAS,40 SOS1,41,42 and RAF1.43,44 These genes are all components of the RAS-MAPK signal transduction pathway that function in regulation of the pathway; any pathogenic mutations are gain-of-function and result in an increase of RAS signaling.41 Gain of function missense mutations in KRAS are present in approximately 1–3% of patients with Noonan syndrome;40,45,46 children with this mutation are reported to suffer from more severe delays in cognition and development than children with Noonan syndrome who lack this mutation.40,45 Mutations in SOS1 cause an estimated 10% of Noonan syndrome; affected children with this mutation have been proposed to be less likely to have short stature and cognitive delays, but more likely to have ectodermal abnormalities such as facila keratosis pilaris.42 Mutations in the most recently identified gene, RAF1, occur in Noonan syndrome in a range of 3–17%; this mutation is associated with a high incidence of hypertrophic cardiomyopathy (80%).43,44
It is now clear that Noonan syndrome shares many phenotypic similarities with other disorders such as LEOPARD syndrome, cardio-facio-cutaneous (CFC) syndrome, Costello syndrome, and neurofibromatosis type 1 (NF1), all of which have a high incidence of some form of congenital heart disease and share germline mutations in the RAS-MAPK pathway. The shared phenotypic features have led some researchers to suggest an umbrella term of neuro-cardio-facio-cutaneous syndromes for all of these disorders.47 LEOPARD syndrome shares many features similar to Noonan syndrome, with the main distinguishing characteristic of lentigines. While Noonan syndrome most frequently has pulmonary valve stenosis and less commonly hypertrophic cardiomyopathy, LEOPARD syndrome has a very high incidence of hypertrophic cardiomyopathy. Mutations in PTPN11 have also been found in patients with LEOPARD syndrome, suggesting that there are distinctive missense mutations in the PTPN11 gene that give rise to the variable incidence in hypertrophic cardiomyopathy and cutaneous findings of lentigines.39 Recently, the mutation in RAF1 has been shown to account for about 10% of cases of LEOPARD syndrome.43 Although CFC syndrome is difficult to distinguish from Noonan syndrome in infancy, the phenotype shows considerable differences with age, and is associated with significant mental retardation and prominent cutaneous manifestations.48,49 Notably, the SOS1 mutation contributing to Noonan syndrome has cutaneous manifestations that may overlap with those seen in CFC syndrome. In 2006, investigators found an association between CFC syndrome and gain-of-function mutations in BRAF, KRAS, and mitogen-activated protein/extracellular signal-regulated kinase (MEK1 and MEK2), all components of the RAS-MAPK pathway.48,50,51 Cardiovascular malformations are frequent in CFC syndrome, and both pulmonary stenosis and hypertrophic cardiomyopathy occur. Costello syndrome can be difficult to distinguish from Noonan syndrome in infancy as well, but does have some facial features that are distinctive from Noonan syndrome or CFC syndrome. Furthermore, malignancies are a significant risk in Costello syndrome: germline mutations in the HRAS gene, belonging to the Ras family and also part of the RASMAPK pathway, were found to be a cause of Costello syndrome.52 The Noonan phenotype has also been associated with patients with neurofibromatosis: one study estimated that approximately 10% of patients with neurofibromatosis have a phenotype similar to that of Noonan syndrome.53 It is likely that the variable phenotypes of the NF1 Noonan syndrome spectrum represent variants of the NF1 mutation in the majority of cases.54 The phenotypic similarities and
isturbances of the RAS-MAPK pathway among these aptly named neuro-cardio-facio-cutaneous syndromes are indicative of this pathway’s important role in development. Greater understanding of these mutational effects on the pathway could lead to better understanding of how the individual phenotypic features arise and better application of current medical therapies to certain post-natal effects, such as impaired growth and cardiovascular complications.
Conclusion
Children with Noonan syndrome are afflicted with cardiovascular, hematological, and muscular problems, in addition to a distinct physical appearance and, in most cases, learning disabilities. The majority, however, will grow up and function quite normally in the adult world. There is still much to learn about the natural history of Noonan syndrome. Close follow-up of patients with the neuro-cardio-faciocutaneous syndromes as they age may be helpful in our understanding of how the RAS-MAPK pathway affects the development and aging process of these patients. With continued research, it is hopeful that we may someday be able to alleviate or at least modify the adverse effects these germline mutations play in development.