Type 2 diabetes (T2D) is a major risk factor for cardiovascular diseases (CVDs) such as stroke, myocardial infarction (MI) and peripheral vascular disease, as well as an independent risk factor for heart failure (HF).1,2 Patients with T2D and established CVD have a substantial reduction of life expectancy (for example, a 60-year-old man with CVD and T2D has a 12-year reduction compared with individuals without diabetes).2 The prognosis for patients with comorbid HF and T2D is particularly poor, with a median survival of about 4 years.3
CVD prevention in patients with diabetes starts with the aggressive reduction of CVD risk factors. The Steno-2 study evaluated an intensive risk factor management strategy including lifestyle changes, as well as blood pressure (BP), lipid and glycaemic control in patients with T2D at high CVD risk.4 The study showed that more intensive risk factor management halved the occurrence of adverse CVD outcomes. A long-term follow-up of the Steno-2 patients showed that life expectancy was more than 7 years longer in patients in the more intensively managed group.4 Studies that have compared intensive glucose lowering with a less intensive strategy over a period of <5 years have not shown consistent reductions of CV events.5–10 Moreover, the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial was prematurely terminated because of increased mortality in the group receiving intensive blood glucose control.11 In extension long-term follow-up studies of ACCORD and Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE), early intensive glucose control was associated with a later improvement in CV outcomes, including a reduction of CV mortality long after the treatment allocation had ended.11,12
For individual glucose-lowering agents, until recently only subsidiary studies or secondary outcomes had shown CVD benefit. In a small sub-study of the United Kingdom Prospective Diabetes Study (UKPDS) of 342 overweight patients with T2D, intensive glucose-lowering with metformin compared with dietary restrictions alone, reduced the risk of MI and all-cause death after 10 years.13 In the PROspective pioglitAzone Clinical Trial In macroVascular Events (PROACTIVE) study of pioglitazone in high-risk CVD patients, the study result was neutral, as the multicomponent primary endpoint was not significantly reduced. Yet the more conventional outcome (a secondary endpoint) of CV mortality, non-fatal MI and stroke was reduced by 16% (hazard ratio [HR], 0.84; 95% confidence interval [CI]: 0.72, 0.98; p=0.027).5
The 2015 Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes (EMPA-REG OUTCOME) study with the sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin was the first glucose-lowering clinical trial to show a significant reduction of the primary CV endpoint.14 Since then, three further studies with diabetes agents have demonstrated significant reductions of the 3-point Major Adverse Cardiac Events (MACE) outcome: with the glucagon-like peptide-1 (GLP-1) agonist semaglutide (Cardiovascular and Other Long-term Outcomes With Semaglutide in Subjects With Type 2 Diabetes [SUSTAIN-6] study), liraglutide (Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome Results [LEADER] study), and with the SGLT2 inhibitor canagliflozin (Canagliflozin Cardiovascular Assessment Study [CANVAS] study).7,14–16
Sodium-glucose cotransporter 2 and glucose homeostasis
The SGLT2 is found almost exclusively in segment one of the proximal tubule and is a high-capacity, low-affinity transporter, which reabsorbs filtered glucose and sodium in equimolar amounts.17 Under physiological conditions, glucose reabsorption by SGLT2 accounts for about 90% of glucose re-uptake, with SGLT1 transporters reabsorbing the residual glucose in segment three of the proximal tubule.17–19
In hyperglycaemic conditions, SGLT2 expression is up-regulated, increasing both glucose and sodium reabsorption.20 The SGLT2 inhibitors reduce the capacity of the proximal tubule to reabsorb glucose, resulting in urinary glucose excretion. The urinary glucose loss lowers blood glucose and consequently reduces glycosylated haemoglobin (HbA1c) and insulin levels.21 As the mechanism of glucose lowering is independent of insulin action, SGLT2 inhibitors can be combined with all classes of glucose-lowering agents, with a low incidence of hypoglycaemia.22 Beyond glycaemic control, the clinical effects of the SGLT2 inhibitors reduce BP, decrease body weight and visceral adiposity and reduce albuminuria and circulating uric acid levels.
Currently, there are four SGLT2 inhibitors approved in Europe and the US for the treatment of T2D as an adjunct to diet and exercise to improve glycaemic control; these include empagliflozin, canagliflozin, dapagliflozin and ertugliflozin.23–29 The main pharmacological difference between the agents is their specificity for the SGLT2 versus SGLT1 cotransporters: empagliflozin 1:5000; ertugliflozin >1:2000; dapagliflozin >1:1400; canagliflozin >1:160.30–33
The Empagliflozin, Cardiovascular Outcomes and Mortality in Type 2 Diabetes (EMPA-REG OUTCOME) study
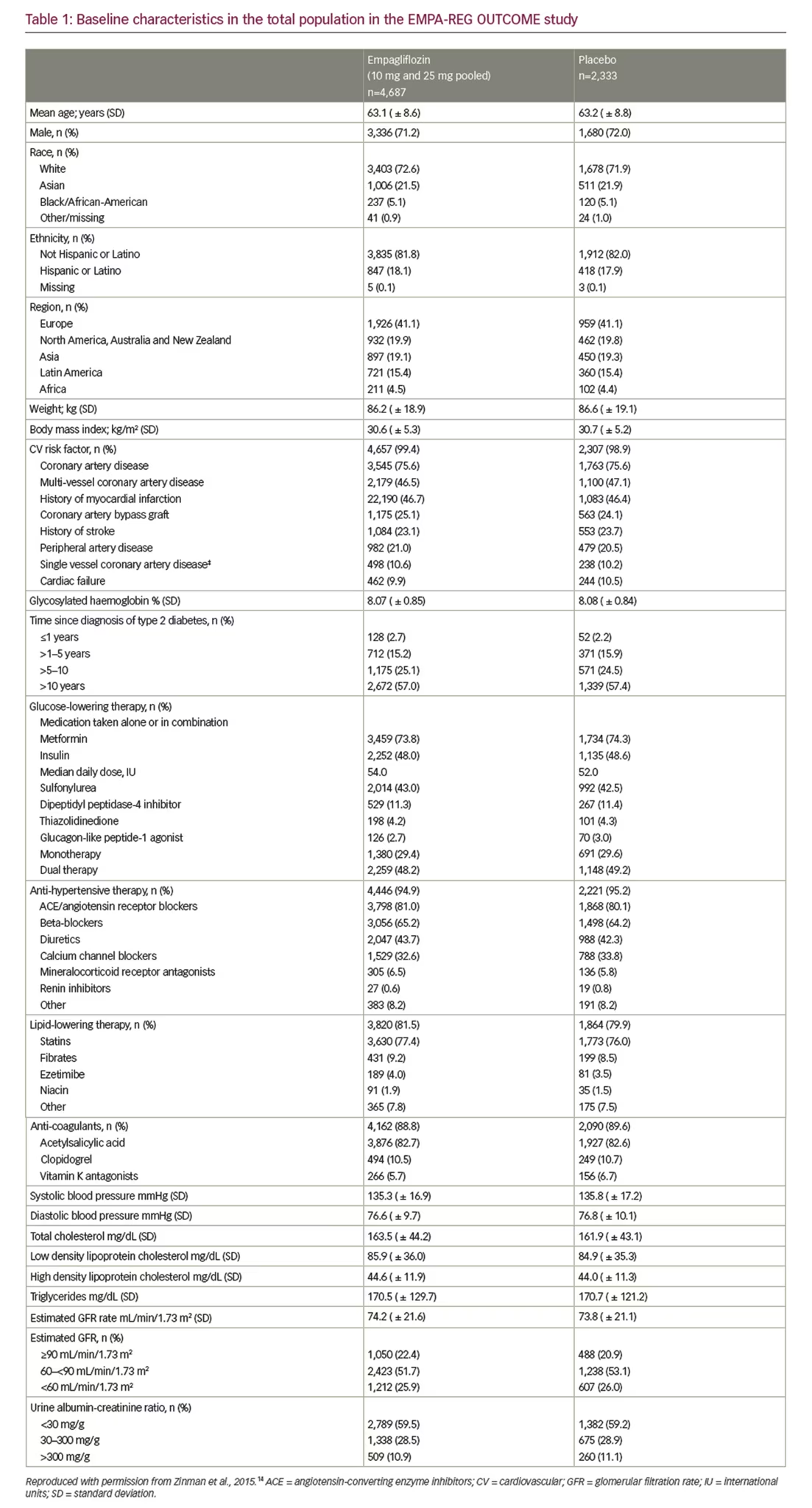
The EMPA-REG OUTCOME study was a multicentre, randomised, double-blind, placebo-controlled study of empagliflozin in patients with T2D and established CVD. A total of 7,028 patients from 42 countries were randomised to receive one of two doses of empagliflozin (10 or 25 mg) or placebo, which was added to optimal care for T2D and CV risk factors. The main statistical analysis was based on the pooled results of the empagliflozin 10 mg or 25 mg groups versus placebo. The median duration of follow-up was 3.1 years.14
Population
The study population at baseline was representative of T2D patients with typical clinical characteristics and current management of T2D and CV risk factors.14 The mean age of patients at study entry was 63 years, the mean body mass index was 30 kg/m2, and just over half of the population had a duration of T2D for >10 years. CVD included multi-vessel coronary artery disease, single vessel coronary artery disease and provokable ischaemia, history of MI, history of stroke and peripheral artery disease (Table 1). A total of 25% of patients had prior coronary bypass surgery and 10% had a history of HF. Anti-hypertensive medications included an angiotensin converting enzyme (ACE)-inhibitor/angiotensin receptor blocker (ARB) (81%), beta-blocker (65%), diuretic (44%) and a calcium channel blocker (33%), and the majority were receiving statins (>76%). Glucose-lowering medications at baseline were metformin (74%), insulin (48%), sulfonylurea (43%), dipeptidylpeptidase-4 (DPP-4) inhibitor (11%), thiazolidinediones (4%) and GLP-1 agonist (3%). The mean baseline HbA1c levels were 8.08% in the placebo group, and 8.07% in the empagliflozin group (Table 1). After the first 3 months’ treatment with either empagliflozin or placebo, investigators were encouraged to adjust glucose-lowering medication to reduce HbA1c levels to locally recommended targets using any choice of glucose-lowering agents. However, many patients did not reach these levels during the study and the adjusted mean HbA1c at week 206 was 7.81% in the empagliflozin group and 8.16% in the placebo group.
Cardiovascular outcomes
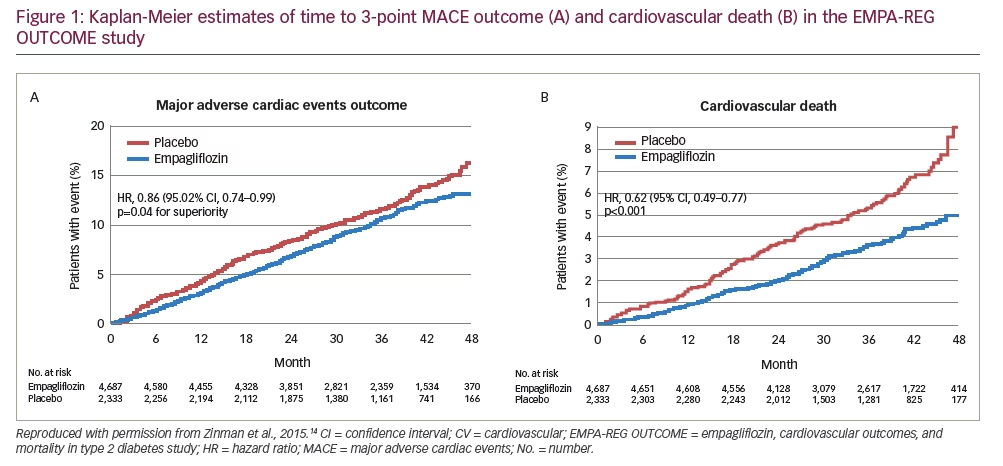
The primary outcome (CV mortality, non-fatal MI and non-fatal stroke) was reduced by empagliflozin (10.5%; 490/4,687) compared with placebo (12.1%; 282/2,333); HR, 0.86 (95% CI: 0.74, 0.99) (Figure 1a). The reduction of the primary outcome was driven by a 38% reduction of CV mortality (HR 0.62; 95% CI: 0.49, 0.77) with no significant reduction of either MI or stroke. The reduction of CV mortality by empagliflozin was seen very early (after less than 3 months treatment) (Figure 1b), and the widening of the difference between the treatment and placebo survival curves indicates an on-going treatment benefit. Empagliflozin also reduced all-cause mortality by 32% (HR 0.68; 95% CI: 0.57, 0.82). The reduction of CV death was observed across a wide range of subgroups such as baseline CVD, gender, age, high or low HbA1c levels, reduction of HbA1C and renal function.14,34,35
Heart failure outcomes
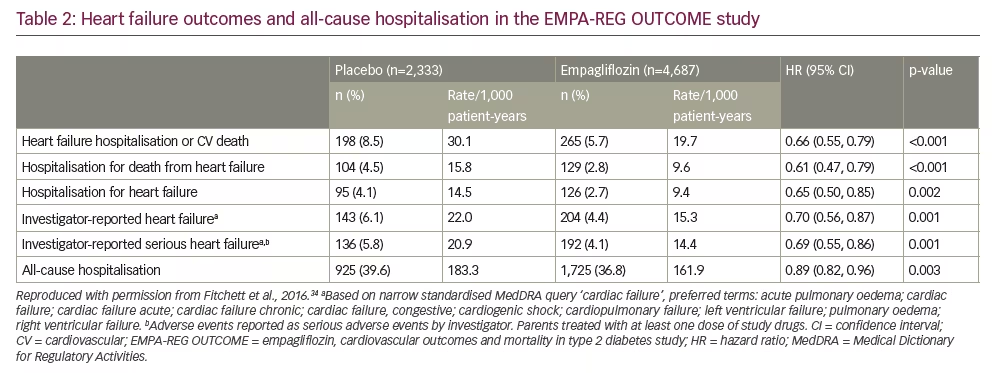
Empagliflozin reduced the adjudicated outcome of HF hospitalisation by 35% (HR, 0.65; 95% CI: 0.50, 0.85). Other non-adjudicated measures of HF outcomes, including investigator-reported HF, the introduction of loop diuretics and death from HF were significantly reduced by empagliflozin (Table 2).34 The rate of HF hospitalisation or CV death was lower for empagliflozin (5.7%) versus placebo (8.5%); HR, 0.66 (95% CI: 0.55, 0.79), with consistent benefits across subgroups including age, race, estimated glomerular filtration rate (eGFR), use of glucose-lowering medication (including insulin), CV medications and diuretics. Among patients who were hospitalised for HF, a smaller proportion receiving empagliflozin died of CV causes (13.5%) than those on placebo (24.2%). Similar reductions of CV mortality and HF outcomes were observed in the 10% of patients with a baseline history of HF as in the overall group.
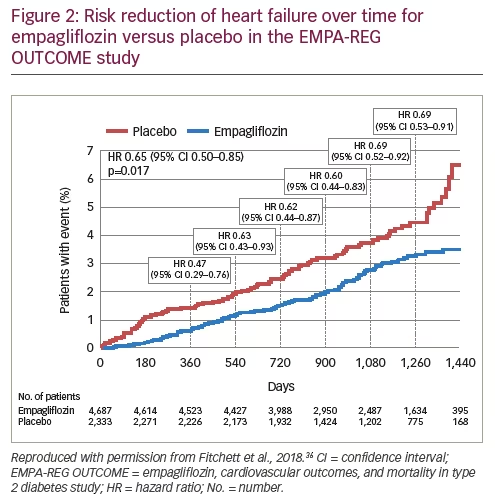
The CV benefits of empagliflozin were also observed in patients across the spectrum of risk for HF.36 In the overall population, using the Clinical Health Aging and Body Composition HF risk score, the reduction in CV death and HF hospitalisation for empagliflozin versus placebo was consistent across the risk subgroups, with a HR (95% CI) of 0.71 (0.52, 0.96) in the low-to-average-risk group, 0.52 (0.36, 0.75) in the high-risk group, and 0.55 (0.30, 1.00) in the very high-risk group; a similar reduction was observed for HF hospitalisation (Figure 2).
A total of 958 (13.6%) patients had a HF burden (HF at baseline, HF hospitalisation or HF reported by the investigator as an adverse event). The rate of CV death was almost four-fold greater in patients with a HF burden, with 38% of all CV deaths in the EMPA-REG OUTCOME trial occurring in this minority group. Although the absolute benefit of empagliflozin was larger (4.9%) in the group with a HF burden (10.4% versus 15.3%, respectively; HR, 0.67; 95% CI: 0.47, 0.97), patients with no HF burden had an important mortality benefit (2.7% versus 4.2%, respectively; HR, 0.63; 95% CI: 0.48, 0.84).
Renal outcomes
Chronic kidney disease (CKD) is a major co-morbidity in patients with T2D, adding to the burden of disease and increasing the risk of death. It is estimated that about 40% of patients with T2D have CKD with urinary albumin/creatinine ratio ≥30 mg/g and/or eGFR ≥60 ml/min/1.73 m2, and 20% of patients with T2D have clinically overt CKD (eGFR <60 mL/min/1.73 m2).37,38 Despite intensive glucose-lowering strategies and the use of renin-angiotensin-aldosterone system (RAAS) agents, patients with T2D remain at increased risk of progressive renal disease, the need for dialysis and renal death.12,39–42
In the EMPA-REG OUTCOME study, the composite renal outcome was the rate of incident or worsening nephropathy defined as progression to macroalbuminuria, doubling of creatinine level, with eGFR of ≤45 ml/min/1.73 m2, the initiation of dialysis, or death from renal disease.35 Incident or worsening nephropathy was reduced with empagliflozin (12.7%) versus placebo (18.8%); HR, 0.61 (95% CI: 0.53, 0.70). The post-hoc renal composite outcomes were: doubling of serum creatinine level, the initiation of renal-replacement therapy or death from renal disease. The risk of these outcomes was reduced for empagliflozin versus placebo by 46%.35 Empagliflozin reduced the risk of progression to macroalbuminuria by 38%, the risk of a doubling of creatinine by 44% and the risk of starting renal-replacement therapy by 55%. Furthermore, from the total population of 7,020 patients, 2,250 (67%) had prevalent kidney disease at baseline defined as eGFR of <60 mL/min/1.73 m2 and/or urine albumin-creatinine ratio (UACR) of >300 mg/g. In patients with prevalent kidney disease, empagliflozin reduced the risk of CV death by 29%, the risk of all-cause death by 24%, the risk of HF hospitalisation by 39% and the risk of all-cause hospitalisation by 19%. These effects were observed across the range of baseline eGFR (<45, 45–<60, 60–<90, ≥90 ml/min/1.73 m2), UACR status (>300, 30–≤300, <30 mg/g) and on top of a high use of RAAS inhibitors (80.7% were taking ACE inhibitors or ARBs).
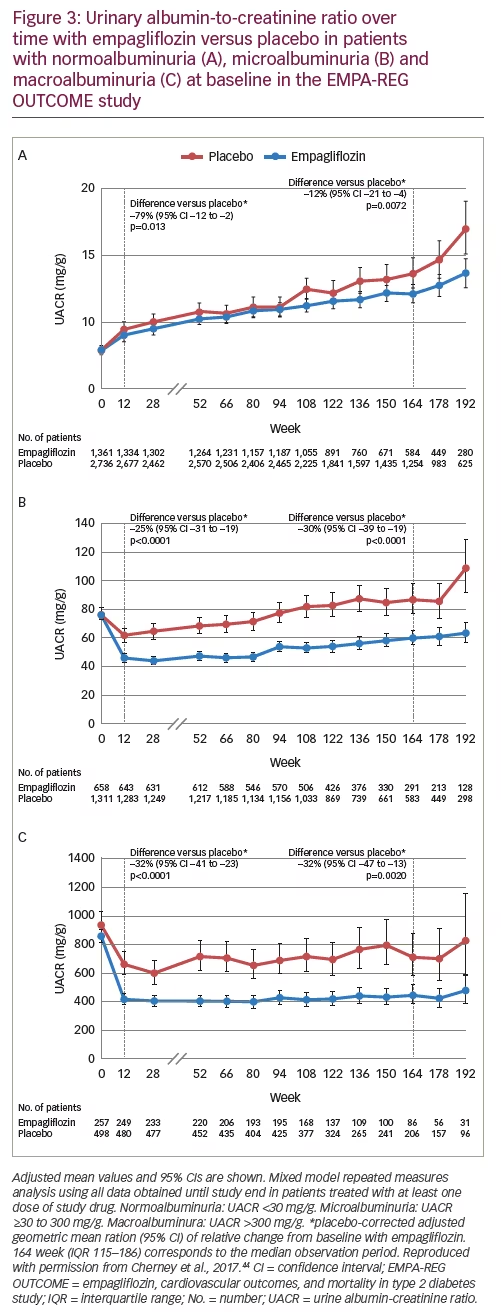
Pre-specified and post-hoc analyses were performed to assess changes in UACR scores, according to baseline UACR status (normoalbuminuria: UACR <30 mg/g; microalbuminuria: UACR ≥30–≤300 mg/g; and macroalbuminuria: UACR >300 mg/g). At baseline, 59% of patients had normoalbuminuria, 29% microalbuminuria and 11% had macroalbuminuria.35,43 In patients with micro- or macro-albuminuria, there was a rapid reduction in UACR with empagliflozin versus placebo that was maintained at week 12 and week 164 (Figure 3).44
The EMPA-REG OUTCOME study – discussion
Improving survival and preventing hospital admission are key goals of the treatment of co-morbid T2D and CVD. In the EMPA-REG OUTCOME study, empagliflozin reduced the risk of CV death by 38%, any cause death by 32% and hospitalisation for HF by 35%.14 Moreover, the rapid improvement in HF outcomes across the spectrum of HF risk with empagliflozin represents a therapeutic advance in the treatment of this poorly recognised major CV co-morbidity in T2D.34,36 The reduction of CV mortality was observed when empagliflozin was given in addition to guideline recommended therapy to reduce CV risk, including statins, ACE inhibitors and ARBs.
The mechanism of action of SGLT2 inhibition for the reduction of CV events is uncertain; however, analyses have shown that improvements in glycaemic control or traditional CVD risk factors such as BP and lipids are unlikely to be involved.45 A mediation analysis indicates that more than 50% of the reduction of CV mortality and reduced HF admission was related to the observed increase in haematocrit.45 The sustained 4% increase of haematocrit observed in patients receiving empagliflozin was likely due to an estimated 7% reduction of plasma volume, which could reduce cardiac loading and might result in improved CV outcomes especially if cardiac function was abnormal.45 Other identified mediators were the reductions of uric acid and albuminuria. Although mediation analysis does not prove causality, it provides targets for future investigation.45 Other possible mechanisms of action include the increased availability of ketone bodies which may be a more efficient fuel for the stressed myocardium than free fatty acids, inhibition of the sodium hydrogen exchanger and modulating the effect of lectins.46–48
T2D is an independent risk factor for HF, with rates of death and hospitalisation in patients with T2D and HF more than 50% greater than in patients without diabetes.3,49–51 In a Swedish study of HF patients with T2D (8,809) and without T2D (27,465), the median survival time was 3.5 years versus 4.6 years, respectively, and the adjusted odds ratio for death was 1.60 (95% CI: 1.50, 1.71).52 Furthermore, certain glucose lowering agents increase the risk of developing HF.11 In contrast, both in patients with and without a history of HF, empagliflozin reduced a range of HF outcomes.53 It is unknown whether these benefits occurred in patients with abnormal cardiac function or elevated Brain Naturetic Factor levels. Consequently, it is uncertain whether empagliflozin is beneficial in patients with HF with either preserved ejection fraction (HFpEF), or with reduced ejection fraction (HFrEF). In addition, it is not yet known whether empagliflozin is beneficial and safe in patients with established HF. Two phase III clinical trials are currently ongoing to assess empagliflozin in patients with either HFpEF or HFrEF and including patients with and without T2D (NCT03057977 and NCT03057951). Both trials will assess empagliflozin versus placebo for the prevention of CV death and HF hospitalisation and are expected to report in 2020.
In the analysis of renal outcomes, empagliflozin reduced the progression of nephropathy and death from renal disease, including in patients with prevalent kidney disease at baseline.35 The modest reduction of BP may have played a small role in preserving renal function. However, it is also possible that modulation of tubuloglomerular feedback by empagliflozin is important. In patients with diabetes, glomerular hypertension and hyperfiltration results from afferent glomerular arteriolar dilatation and efferent arteriolar constriction.54 The precise mechanism of the glomerular hemodynamic abnormalities is not yet defined.55 SGLT2 inhibition increases tubular sodium concentration which is sensed by the macula densa. Adenosine released by the macula densa constricts the afferent glomerular arteriole reducing glomerular hypertension and hyperfiltration, consequently stabilising renal function.56
Empagliflozin – safety and tolerability
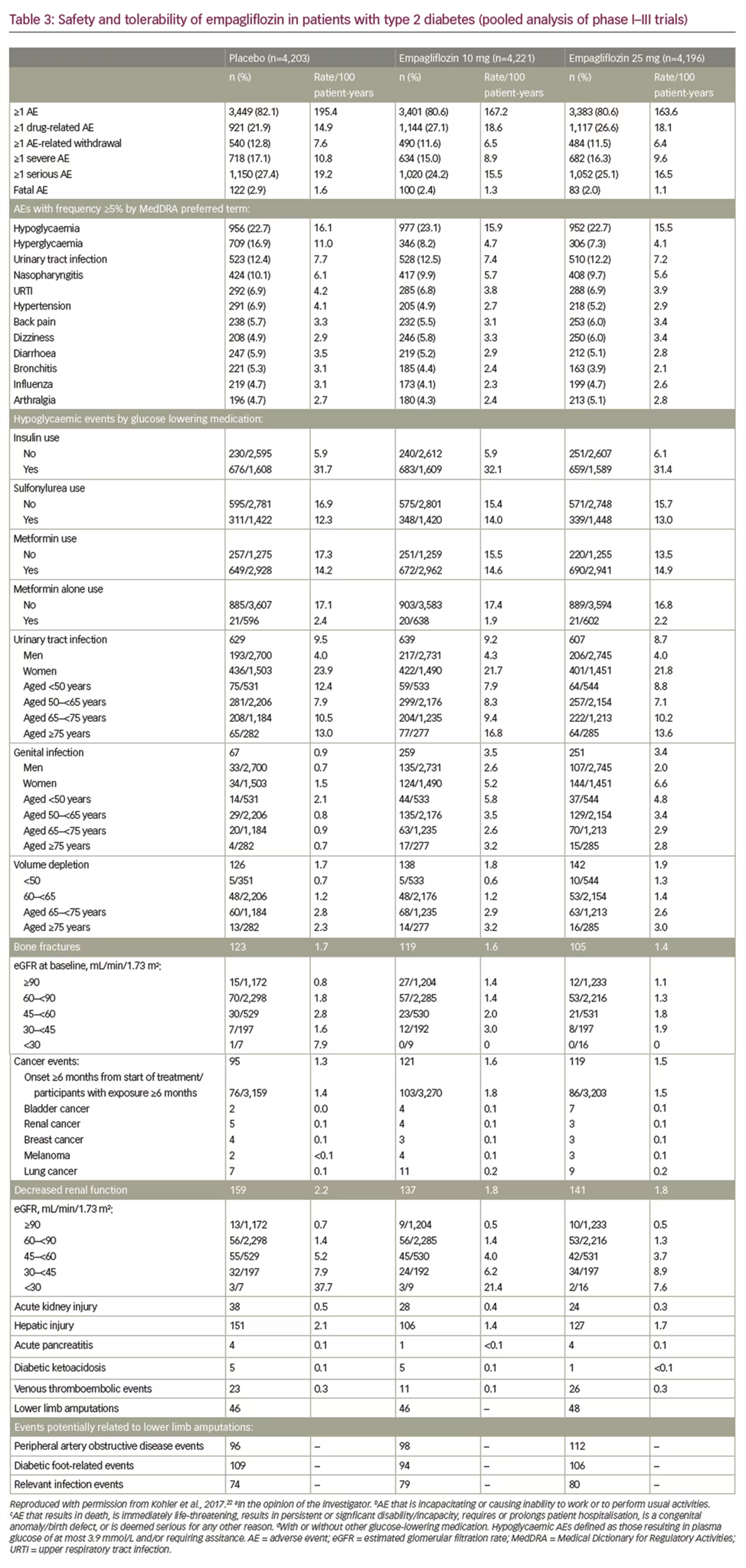
The safety and tolerability of empagliflozin was recently assessed in a pooled analysis of 15 trials, and four extension studies including patients treated with empagliflozin 10 mg or 25 mg (n=4,221 and n=4,196, respectively), or placebo (n=4,203).22 The study showed that the incidence of confirmed hypoglycaemic events was similar for empagliflozin and placebo as an add-on to insulin or metformin with or without other glucose-lowering medication, yet the incidence of hypoglycaemia was higher when empagliflozin was added to sulfonylureas (Table 322). Urinary tract infections (UTIs) were more common in women than men, with a similar incidence in the empagliflozin and placebo groups for both sexes (Table 3). The incidence of complicated UTIs, such as pyelonephritis, urosepsis or serious adverse events consistent with UTI, was 0.6% and 0.9% for empagliflozin 10 or 25 mg, respectively, and 0.9% for placebo. Genital mycotic infection was increased in both sexes and was more frequent in women than men (Table 414,16,57,58); however, infections were usually easy to treat and less than 10% of patients developing a genital infection had to discontinue treatment with empagliflozin.22 Furthermore, genital infections may be reduced by good perineal hygiene.
In the EMPA-REG OUTCOME trial, other safety adverse outcomes were not increased by empagliflozin including bone fractures, cancer events, renal adverse events (including acute kidney injury), thromboembolic events, hepatic injury, acute pancreatitis, lower limb amputations and diabetic ketoacidosis.14
Empagliflozin – place in therapy
Indications
Empagliflozin was licenced in 2014 in the US and Europe as a treatment for adults with T2D, and indicated as an adjunct to diet and other glucose-lowering agents to improve glycaemic control.27,28 In 2016, the FDA approved empagliflozin for the reduction of CV death in adult patients with T2D and CVD. In Europe, the EMA recognise the results of the EMPA-REG OUTCOME study and the reduction of CV mortality with empagliflozin.
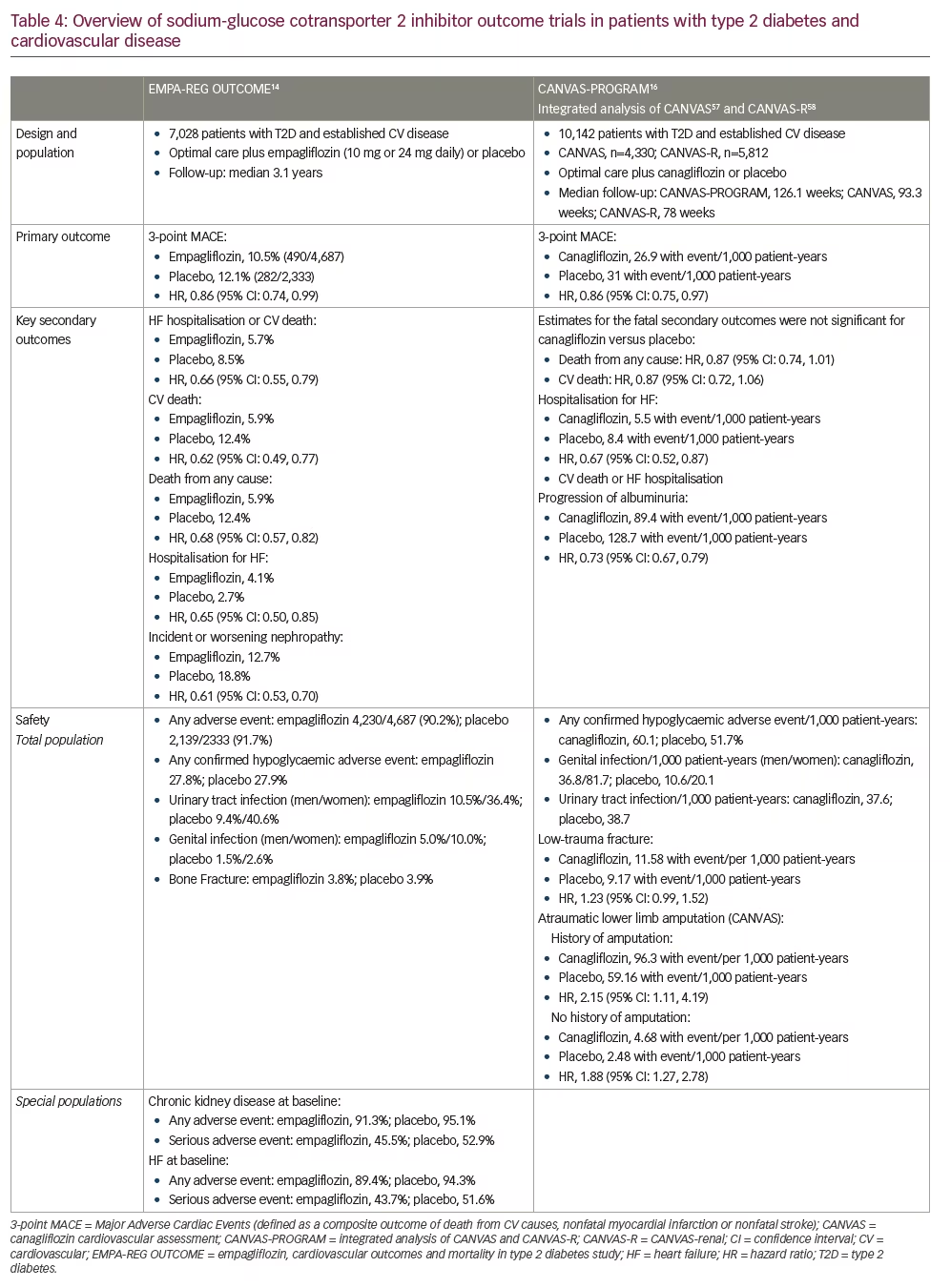
The SGLT2 inhibitors canagliflozin, dapagliflozin and ertugliflozin are approved to lower blood sugar as an adjunct to diet and exercise.23–29 In the CANVAS study, canagliflozin was shown to improve CV outcomes in patients with T2D and CV risk factors, with a 14% reduction of the primary 3-point MACE outcome.16 However, unlike empagliflozin, canagliflozin did not reduce either CV or all-cause mortality.16 Both empagliflozin and canagliflozin reduced HF hospitalisation and improved renal outcomes.16 An overview of the primary, key secondary and safety outcomes in EMPA-REG OUTCOMES study and CANVAS study are shown in Table 4.
Glycaemic control
During pre-registration phase III development, empagliflozin was assessed in several randomised controlled trials for the reduction of HbA1c versus placebo, sitagliptin, glimepiride, linagliptin and metformin.59–70 Patients received empagliflozin as add-on to metformin,59 metformin + sulfonylurea,60 pioglitazone ± metformin,61 basal insulin,62 multiple daily injections of insulin63 or were drug-naïve/pre-treated with any oral anti-diabetes therapy.64,65
Reductions in HbA1c levels from baseline to 12–24 weeks were greater for empagliflozin versus placebo, and empagliflozin also reduced BP and improved weight loss versus placebo.59–65 However, it should be noted that reductions in HbA1c depend upon baseline levels; patients with baseline HbA1c 10.0% can expect about a 2% decrease, whereas from a starting point of HbA1c 7.5%, reductions were more modest at about 0.5%.59–65 In a study of empagliflozin versus glimepiride, both added to metformin, reductions in HbA1c levels were similar between groups, although glimepiride was associated with weight gain (mean 1.6 kg), and empagliflozin was associated with weight loss (mean −3.2 kg).69
The results of ten phase III trials of empagliflozin in patients with T2D were analysed in a recent systematic review which reported that when used as an add-on treatment to metformin, empagliflozin improved long-term HbA1c levels compared with glimepiride, and had a similar effect as linagliptin and sitagliptin.71 The analysis also showed that the combination of metformin and empagliflozin was well-tolerated with minimal hypoglycaemia.
Clinical guidelines
The American Diabetes Association (ADA) and Diabetes Canada guidelines recommend that either empagliflozin or liraglutide should be considered in patients with T2D and established CVD.72–4 The Canadian Diabetes Association (CDA) treatment guidelines (2016) recommend that for patients in whom glycaemic targets are not met, empagliflozin or liraglutide should be added to metformin as the optimal second-line choice to reduce the risk of CV death.74 Empagliflozin is recommended by the European Society of Cardiology (ESC) Heart Failure guidelines for the prevention of HF and reduction of CV mortality in patients with diabetes and established CVD. The ESC guidelines for CVD prevention in clinical practice state that, ‘empagliflozin demonstrated substantial reductions in CV death (by 38%) and all-cause mortality (by 32%), as well as hospitalisation for HF (by 35%), as compared with standard care, suggesting use of an SGLT2 inhibitor should come very early in the course of management of patients with diabetes mellitus and CV disease’.75,76
Conclusions
In patients with T2D, modulation of glucose-handling by the kidney with SGLT2 inhibitors lowers HbA1c levels, decreases body weight and visceral adiposity and improves cardio-renal haemodynamics. Currently, four SGLT2 inhibitors are approved in the US and Europe to improve glycaemic control. Empagliflozin is the only SGLT2 inhibitor that is indicated to reduce the risk of CV death in adults with T2D and CVD. In the overall population, and across a wide range of baseline subgroups such as HbA1c level, renal function (down to eGFR 30 ml/min/1.73 m2) and HF risk, empagliflozin reduced the risk of CV death, all-cause death and hospitalisation for HF. These findings suggest that empagliflozin should be considered in patients with T2D and CVD to reduce the risk of CV and all-cause death.







