This concentration gradient may be more than 100:1 in a hyperactive thyroid, as seen in patients with Graves’ disease. The daily intake of an adult human varies from less than 10mg in areas of extreme iodine deficiency to several hundred milligrams for some people receiving medicinal iodine.
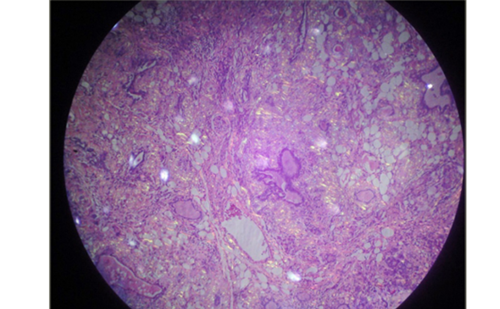
This concentration gradient may be more than 100:1 in a hyperactive thyroid, as seen in patients with Graves’ disease. The daily intake of an adult human varies from less than 10mg in areas of extreme iodine deficiency to several hundred milligrams for some people receiving medicinal iodine. Too little iodine causes menta retardation, goitre, hypothyroidism and other features of the so-called iodine deficiency disorders (International Council for Control of Iodine Deficiency Disorders current iodine deficiency disorders status database –http://www.iccidd.org). Too much iodine increases the incidence of iodine-induced hyperthyroidism, autoimmune thyroid disease and perhaps thyroid cancer. The appropriate intake is about 150mg/day.Iodide entering the thyroid gland must sequentially cross two lipid bilayers the basolateral and then the apical plasma membrane of polarised thyroid epithelial cells or thyrocytes forming the functional units of the gland, the follicles. Thyroid follicles are made of a single layer of polarised cells delimiting a closed internal compartment.
Once in the lumen of follicles, iodide is used to generate iodothyronine residues inside thyroglobulin molecules for the subsequent production of free thyroid hormones. As with other small charged molecules, iodide cannot easily diffuse through cell membranes; thus, its transfer from one side to the other of the thyroid cell plasma membrane requires a membrane proteinThe protein ensuring the active transport of iodide at the basolatera plasma membrane of thyrocytes (named NIS for Na+/iodide symporter) is now well characterised.1 The movement of iodide from the cytoplasm of thyrocytes to the follicle lumen is expected to be a passive process; indeed, due to the favourable electrochemical gradient, iodide efflux would require only a ‘permease’ or an ion channel. The transport of iodide from the cytoplasm of thyrocytes to the follicle lumen has been elegantly studied on polarised porcine thyrocytes cultured as tight monolayers in bicameral devices;2 it was reported that the apical efflux of iodide, which is rapidly increased in response to thyroid-stimulating hormone (TSH), could occur through a cyclic adenosine monophosphate (cAMP) regulated ‘iodide channel’. A study performed on thyroid membrane vesicles3 also concluded that an iodide channel must exist in the thyroid. Molecular identification of the protein ensuring the transport of iodide at the apica membrane of thyrocytes has been the goal of several recent studiesPendrin, the protein encoded by the gene altered in Pendred’s syndrome (PDS), i.e. the PDS gene, has been the first candidate. Pendrin, a membrane protein located at the apical pole of thyrocytes, is endowed with ion transport activity.Pendrin was rapidly considered as the apical iodide transporter despite the uncertainties and/or discrepancies that were apparent since the first reports. The initial proposal of pendrin as a sulphate transporter4 was rapidly abandoned.5 Most subsequent studies performed on different experimental systems assigned a function of anion exchanger to pendrin, exchanging chloride for hydroxide, bicarbonate or formate;5–9 some studies based on transfection of recipient cells concluded that pendrin could be active as a chloride/iodide transporter10–11 or chloride/iodide exchanger.12It is difficult to envisage any physiological contribution from a chloride/iodide exchanger in the apical iodide efflux, since both uminal and cytoplasmic chloride concentrations are more than 1,000-fold greater than that of iodide; an exchange of cytoplasmic iodide with luminal chloride on a one-to-one stoechiometry seems unlikely Still more confusing are the reports claiming that pendrin mediates iodide uptake (not efflux) by MCF-7 cells.13 At present, there are no experimental data showing that pendrin activity accounts for the ‘transfer’ of iodide from thyrocytes to the apical compartment in a polarised thyroid cell system.
Data from polarised Madin-Darby canine kidney cells transfected with the PDS gene,14 although interesting, should not be extrapolated and considered as a demonstration of the function of pendrin in the thyroid. Several other arguments undermine the hypothesis of pendrin as an apical iodide transporter. First, the knockout of the PDS gene in the mouse, which causes functiona alterations in the ear, does not induce any thyroid phenotype.15Second, it has often been found that many patients with Pendred’s syndrome who have a non-functional pendrin do not exhibit any thyroid alteration. Third, it seems difficult to accept that a given protein could have different functions in different organs. In the thyroid, pendrin – SLC26A4 in the solute carrier (SLC) transporter nomenclature – could exert a function of chloride/bicarbonate exchange (as in the kidney) and play, for example, a role in the control of luminal pH with a possible incidence on iodide oxidation indecision about the identity of the apical iodide transporter has been complicated by a report describing another candidate named apica iodide transporter (AIT).16 As with pendrin, AIT appears selectively located at the apical plasma membrane of thyrocytes and, as with pendrin, was reported to cause iodide discharge in transfected cell systems. The first problem arose when it was found, using colon cell lines, that this protein – structurally related to NIS – was an Na+-dependent transporter17 belonging to the SLC5 family as the SLC5A8 member. Indeed, both previous studies and prediction on biological considerations do not point to the requirement for an Na+ dependency for the apical iodide transport. Soon after, two independent groups described SLC5A8 as an Na+-coupled transporter for short-chain fatty acids. 18–20 Recent studies on SLC5A8 indicate a consensus on this function.21–23 Attempts to detect an activity of SLC5A8 in iodide efflux have been unsuccessful.23
At this stage, one has to conclude that the identity of the protein(s) ensuring the apical iodide transport in the thyroid is not known.