The prevalence of overweight and obesity has increased worldwide over the last 30 years.1–5 It was estimated that in 2005, 23.3 % of the world population was overweight and 9.8 % was obese6 and in 2009–10, 37 % of adults in the US and almost 17 % of youths were obese.7 Predictions concerning overweight and obesity prevalence suggest that the majority of the world’s adults will be overweight or obese by 2030. In the US, it is estimated that 86.3 % of adults will be overweight and 51.1 % will be affected by obesity.8
The prevalence of overweight and obesity has increased worldwide over the last 30 years.1–5 It was estimated that in 2005, 23.3 % of the world population was overweight and 9.8 % was obese6 and in 2009–10, 37 % of adults in the US and almost 17 % of youths were obese.7 Predictions concerning overweight and obesity prevalence suggest that the majority of the world’s adults will be overweight or obese by 2030. In the US, it is estimated that 86.3 % of adults will be overweight and 51.1 % will be affected by obesity.8
Obesity and its associated health risks involve direct and indirect economic costs that impact significantly on healthcare systems. In the US, these costs were estimated at $147 billion in 2008. Heathcare costs are predicted to double every decade, reaching about $956.9 billion in 2030.9There is, therefore, a critical need for global strategies to prevent obesity.
A growing body of evidence shows that prevention through a lifestyle modification in eating habits and physical activity is one of the most efficient and cost-effective ways to tackle the obesity epidemic.10 Furthermore, lifestyle modification is associated with substantial risk reductions for metabolic diseases; a recent epidemiologic study found that individuals undertaking regular physical activity had a reduced risk for Type 2 diabetes (T2D): odds ratio (OR) 0.76 for men (95 % confidence interval [CI] 0.73–0.79) and 0.77 for women (95 % CI 0.73–0.82).11
In order to be effective, public interventions for the prevention of obesity should be implemented in three stages: targeting entire populations, highrisk subgroups of the population, and individuals at high risk. This may be undertaken at national, state, and community levels, and should involve numerous sectors, such as childcare facilities, schools, workplaces, and seniors centers. A focus on specific populations may be required to ensure that interventions address disparities in social and environmental conditions related to food consumption and physical activity. A positive correlation has been demonstrated between low-socioeconomic status and obesity. A review of studies conducted in 13 EU member states suggested that over 20 % of the obesity in European men and over 40 % of the obesity in women was attributable to socioeconomic inequalities. In addition, obesity among children was associated with the socioeconomic status of their mothers.12
Public interventions targeting obesity have had varying degrees of success; however, a community-based intervention, the Fleurbaix Laventie Ville Santé Study (FLVS), demonstrated significant reductions in the prevalence of both overweight and obesity and in health inequalities.13This long-term intervention pilot program formed the basis of the Ensemble, Prévenons l’Obésité des Enfants (EPODE) methodology, disseminated today in more than 17 countries. This article’s aim is to outline the EPODE methodology, to discuss its potential for transferability, and to suggest ways in which EPODE may be used as a model for future strategies to reduce the global incidence of other weight-related comorbidities.
Health Effects of Overweight and Obesity
Overweight and obesity in childhood are known to have significant impacts on both physical and psychologic health and both are associated with abnormal glucose tolerance and an increased risk of T2D. Moreover, adipose tissue releases nonesterified fatty acids, glycerol, hormones and pro-inflammatory cytokines, all of which are associated with the development of insulin resistance.14 T2D has become a global epidemic and is associated with increased risk of cardiovascular disease (CVD) and premature mortality. Between 1980 and 2006, the number of adults with T2D rose from 153 million to 347 million worldwide.15
Obesity and overweight can result in numerous other adverse health outcomes, including dyslipidemia, hypertension, coronary artery disease, certain cancers, sleep apnea and an increased risk of mortality.16 In children, overweight has been associated with T2D, sleep apnea, hypertension, dyslipidemia, the metabolic syndrome, and psychologic disorders such as depression.17 Overweight children subsequently monitored in later life had increased incidence of CVD, digestive diseases, and all-cause mortality compared with those who were lean.18,19
The EPODE Methodology
The EPODE methodology is the result of a study that was initiated in 1992 in two towns in northern France (Fleurbaix and Laventie). The FLVS study was a long-term school-based intervention followed by a communitybased program. Actions included in the intervention aimed to improve eating and physical activity habits among children.13 Initial data obtained from this study showed that interventions solely targeting schools were not sufficient to significantly reduce the prevalence of obesity and overweight (see Figure 1). Improved results were obtained through a subsequent community-based intervention that involved many local stakeholders.13 Evaluation of the results of this study led to the identification of the main factors of success that formed the basis of the EPODE methodology.
EPODE is a coordinated, capacity-building approach aimed at reducing childhood obesity through a societal process in which local environments, childhood settings, and family norms are directed and encouraged to facilitate the adoption of healthy lifestyles in children (i.e. the enjoyment of healthy eating, active play, and recreation).20 The primary EPODE target groups are children from 0 to 12 years old and their families. The programs based on the EPODE philosophy are long-term, aimed at changing the environment and thus unhealthy behaviors. The approach to healthy lifestyle habits is positive, and does not stigmatize any culture, individual, food habit, or behavior. Messages and actions are tailored to the target population (e.g. according to age, socioeconomic status, etc.)
The FLVS study identified four critical factors that form the four main pillars of the EPODE methodology.20,21 The first is political commitment: formal commitment is sought from political representatives from the local community to the state and federal level. The second is securing sufficient resources to fund central services, as well as contributions from local organizations to fund implementation at the community level. The third is planning, coordinating actions, and providing the social marketing and support services at community level. The last pillar uses evidence from
Figure 1: Evolution of Children Obesity Prevalence in the Towns in EPODE and in Comparison Towns Between 1992 and 200413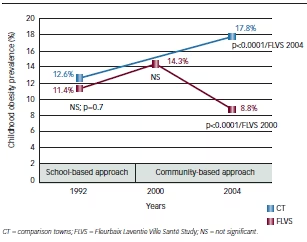 numerous sources to guide the implementation of EPODE interventions and to evaluate outcomes.
numerous sources to guide the implementation of EPODE interventions and to evaluate outcomes.
The community-based interventions based on EPODE methodology are evaluated following their four levels of implementation: central and local organization levels, setting level, and child level.20,21 Evaluation includes both process and outcomes indicators monitoring. The heights and weights of children from the age of five to 12 are measured, and body mass index (BMI) calculated and recorded on a spreadsheet. Although the accuracy of BMI in diagnosing obesity is limited,22 it allows international comparisons, and is therefore preferred among other adiposity markers in children. Changes in food and physical activity habits are assessed by specific questionnaires administered in schools or other settings (e.g. local health centers). These data are submitted to the local project manager, who disseminates the results. Actions implemented at local level are evaluated by interviews and questionnaires that are also submitted to the local project manager.
The evaluation framework is designed by the central coordination team, with the expertise of a scientific committee and feedback from local stakeholders. Evaluation is a key-driver for politicians and fosters mobilization of stakeholders in a sustainable way. It also allows media coverage of the program by highlighting the activities carried out, which motivates the target population.
The EPODE methodology relies on the importance of political awareness, willingness, and involvement to set-up and implement EPODE initiatives. Political representatives have a central role in obesity prevention because they control numerous factors, notably urban development, schools management, catering standards, and they can define priorities in the economic sector.23They are in a position to make obesity prevention a global priority at their level (national, state, or federal), to initiate and support cross-sectoral interventions in communities. In each community the local leader (e.g. the mayor) has to be able to endorse the program.
The EPODE approach promotes the involvement of multiple stakeholders at central level, with endorsements from ministries and support from health
Figure 2: EPODE Methodology—Local and Central Level Multistakeholder Approach
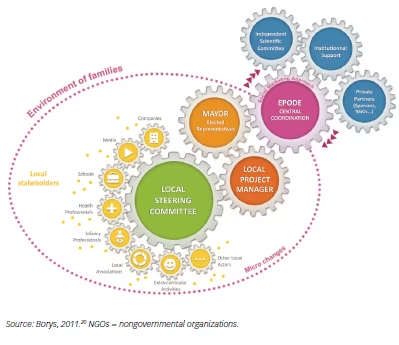
groups, nongovernmental organizations (NGOs) and private partners. A Central Coordination Team (CCT) leads the implementation of programs at community level, by training and coaching local project managers (see Figure 2). The CCT employs social marketing to develop messages, actions, and tools aimed at influencing social and physical environments, informed by evidence and in line with official recommendations. A local project manager aims to mobilize local stakeholders (teachers, local NGOs, catering services, etc.) to form a steering committee.
The global mobilization involved in the EPODE methodology leads to a strong public–private partnership (PPP). Such partnerships are being employed worldwide to address the childhood obesity problem.24,25 Drawing on academic26 and expert definitions,27,28 a PPP can be defined as the cooperation between public and private sectors to work toward shared objectives through mutually agreed division of labor, and by committing resources and sharing the risks as well as the benefits. A PPP requires the involvement of at least one public and one private partner. Most PPPs include partners from the public sector (e.g. governmental agencies), the for-profit sector and the ‘civil society’ (academia and NGOs). In the EPODE community-based experience, the presence of a PPP has been a major factor for success. To be fully effective, the following principles have to be respected: shared objectives between public and private members of the PPP, transparency, formal commitment, balance, patience, and mutual trust. PPP applies to all levels of the EPODE program implementation.
Results of Interventions Based on the EPODE Methodology
Transferability and Sustainability
The EPODE methodology has shown encouraging results in ensuring the sustainability of community-based programs. Since the local community is at the heart of the initiative, the methodology can be modified according to age, socioeconomic group, different cultures, and even different geographical areas. The EPODE methodology is now implemented on a large scale and the number of countries involved in the project continues to increase (see Figure 3).20
By 2012, community-based interventions inspired by the EPODE methodology had been implemented in 17 countries. The South Australian and Mexican Health Ministers adopted the methodology to conceptualize and implement their ‘National plan on nutrition and physical activity’ (Obesity Prevention and Active Lifestyle (OPAL) program and 5 Pasos strategy, respectively).
Moreover, the EPODE methodology has shown great plasticity. It has been applied by private bodies such as the Protein Health Communication in Brussels (coordinating the VIASANO program), by public and private institutions, in the case of the JOGG program (within the Convenant on Healthy Weight) in the Netherlands, and by exclusively public organizations, such as the OPAL program in South Australia, established in 2009, which is run by the Health Ministry of the South Australian Government. These programs have been developed in various contexts in term of culture of the targets, of obesity prevalence, and of political involvement on obesity prevention. Recently a report from the Canadian Healthy Kids panel recommended implementation of the EPODE methodology in Ontario.29
Impact on Overweight and Obesity Prevalence
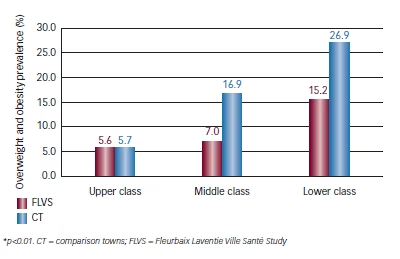
In addition to the global impact on overweight and obesity prevalence, the FLVS study demonstrated that this prevention program was efficient across all socioeconomic levels (see Figure 4).13 Based on the lessons learned from this pilot study, the EPODE methodology was implemented in eight French towns. Children in age groups from four to five and 11 to 12 (n=23,205) were weighed and measured annually between 2005 and 2009 by school health professionals. While national data available in France indicated an overall stabilization in the prevalence of childhood overweight and obesity, results from the eight French EPODE pilot towns showed a significant decrease of 9.12 % (p<0.0001) in overweight and obesity between 2005 and 2009. Encouragingly, children who attended schools in deprived areas showed a downward trend of 2 % (nonsignificant, p=0.38) in the prevalence of childhood overweight (including obesity), compared with an increase in the prevalence of overweight and obesity in children from disadvantaged households at national level.30
The VIASANO program, based on the EPODE methodology, was launched in 2007 and 2008 in two towns in Belgium. During the school year 2007/2008, children in year 1 and 3 of nursery schools (n=1,300) were weighed and measured by the School Health Prevention Services, as well as another 1,484 children in 2009/2010. The prevalence of overweight in nursery school children showed a decrease of 22 % (p<0.05), from 9.46 % to 7.41 %. In the same period in the control towns, the prevalence of overweight slightly increased, from 9.53 % to 9.58 %. These results also provide evidence for the transferability of the EPODE methodology in other settings and culture.31,32
Main Messages of the EPODE Studies Childhood Obesity Prevention is Vital to Preventing Lifestyle-related Diseases
Childhood obesity is responsible for an increased risk of obesity and weight-related disease in adulthood. Indeed, nearly 60 % of obese children will continue to suffer from obesity throughout their adult life.33Currently, no therapeutic medium or drug has proved to be safe and efficient in the treatment of obesity on a long-term basis. Prevention is the most efficient and cost-effective way to tackle the obesity epidemic.34 As a consequence, interventions targeted at children and their families are vital to the prevention of obesity and lifestyle-related diseases. To date, the evaluation is more focused on children’s health outcomes and behaviors but in the future it would be worthwhile to be able to assess the impact of the interventions on adults behaviors related to diet and physical activity.
Relevance of the Community-based Approach
Interventions in the prevention of obesity should consider genetic, behavioral, economic, sociologic, environmental, psychologic, and political factors.35 Community-based approaches tend to involve stakeholders in order to have an impact on the majority of obesity determinants. Modifying the environment in a sustainable manner that makes healthy behaviors the most natural, easy, and rewarding response, is the only effective way to change behaviors. The long-term success of the EPODE and VIASANO programs suggests that community-based interventions can be successfully implemented of a larger scale.
Involvement of Outside Bodies Involvement
of policy-makers, and especially local policy-makers, is crucial to mobilize target populations and change local environments. Indeed, beneficial political consequences may emerge from such a commitment: visibility, positive impacts on public health, no political opposition, and the development of a federative project for the entire community.30 The food and drink industry should also be involved in community-based interventions. A global commitment in the framework of a PPP may lead to a positive evolution in product reformulation, restriction on advertising aimed at children, innovative solutions for a healthier range of products, better employee awareness, or even providing marketing expertise to improve social marketing techniques.
Scientific Data Evaluation Scientific evaluation is an important component of the EPODE methodology. By ensuring that actions implemented meet local needs, evaluation ensures sustainability and allows for optimization of programs and enhanced publicity. However, evaluation is expensive and timeconsuming, requiring at least 15 % of the program budget.36,37 Lessons remain to be learned from deeper evaluations; in particular, there is a need to reach an optimum balance between scientific standards and feasibility. Evaluation has to be useful to all stakeholders, and is a major factor of a sustainable political involvement.
Applicability of the EPODE Methodology to Other Lifestyle-related Disease Prevention
It is widely recognized that community-based interventions such as EPODE create the conditions to enable people to make ‘healthy’ choices and adopt healthy behaviors, and are an efficient means of prevention of childhood overweight and obesity. As a consequence, such interventions should impact on the incidence of other weight-related diseases such as T2D. Further research is needed to implement programs aimed at preventing other lifestyle-related diseases, such as cancers and respiratory failure linked to tobacco use or alcohol-related diseases. According to the United Nations, the combination of four healthy behaviors (balanced
Figure 3: Evolution of the Number of Towns Involved in Community-based Interventions in Six Countries Based on EPODE Methodology20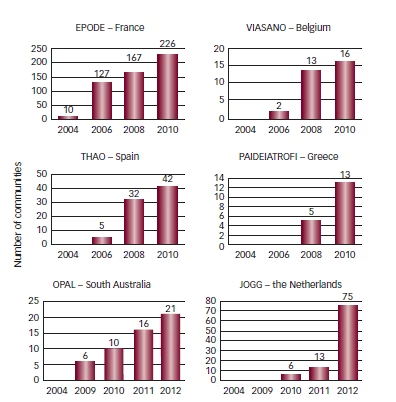
Figure 4: Obesity and Overweight Prevalence (%) According to Socioeconomic Groups in 2004 in EPODE Towns Compared with Comparison Towns13
diet, regular physical activity, keeping a healthy weight, and not smoking) may reduce the risk of developing the most common and deadly chronic diseases by 80 %, with positive social and economic consequences.38
Conclusion
It is important to reverse trends toward increasing obesity by interventions at the community level. The multistakeholder approach promoted through the EPODE methodology has been successful for more than 20 years. Moreover, its implementation on a large scale, through EPODE and EPODElike programs, has led to a significant decrease of overweight and obesity in unselected populations and, importantly, reduced the socioeconomic gap in obesity prevalence in France. The EPODE framework has created political willingness to engage more in obesity prevention.
Despite these advances, there are still significant gaps to bridge between awareness and realities at the grassroots level. Many lessons remain to be learned from the implementation of interventions based on the EPODE methodology in terms of scientific research, evaluation, and longterm funding. There remains a requirement for concrete ways to ensure sustainability of interventions in real-life settings.39 Future interventions should develop more adapted actions and messages targeting lessadvantaged populations. In relation to this specific concern, from 2012 to 2015, the European Commission together with a pan-European consortium will work together to evaluate the added value of the implementation of an adapted EPODE methodology within community-based programs for the reduction of socioeconomic inequalities in health-related diet and physical inactivity behaviors of families with children aged six to nine, living in seven European communities.
To ensure a wider implementation of EPODE-like programs, a deeper evaluation is required. As a consequence, the Epode European Network (EEN) and the EPODE International Network (EIN) have been created to support the worldwide implementation of community-based interventions. The major partners in the EEN program include four committees, each one headed by one of four major European Universities (Amsterdam, Gent, Lille, Saragoza), and four private partners.
These international networks allow the sharing of experience and best practices for the continuous improvement of the programs. The EIN network reflects the worldwide movement to prevent obesity and provides a solution to the advance of weight-related diseases.







